Find Help
More Items From Ergsy search
-

Diagnosing Coeliac Disease Updated 2021
Relevance: 100%
-

Coeliac Disease: Session 1: What is Coeliac Disease?
Relevance: 71%
-

Coeliac disease
Relevance: 71%
-

NHSGGC - What is Coeliac Disease?
Relevance: 65%
-

Causes of coeliac disease
Relevance: 65%
-

Symptoms of coeliac disease
Relevance: 62%
-

Coeliac Disease: The gluten free diet
Relevance: 62%
-

Living Well with Coeliac Disease
Relevance: 61%
-
Coeliac Disease Explained - Gluten Sensitivity - A to Z of the NHS - Dr Gill
Relevance: 54%
-

How is Crohn's disease diagnosed?
Relevance: 38%
-

Diverticular Nov 2021
Relevance: 38%
-

How is Huntington's disease diagnosed?
Relevance: 38%
-

How is Alzheimer's disease diagnosed?
Relevance: 37%
-

How is flesh-eating disease diagnosed?
Relevance: 37%
-

When did the Domestic Abuse Act 2021 come into effect?
Relevance: 36%
-

How is sickle cell disease diagnosed?
Relevance: 36%
-

What tests are available for diagnosing Lyme disease?
Relevance: 35%
-

How is Marburg virus disease diagnosed?
Relevance: 35%
-

How is motor neurone disease diagnosed?
Relevance: 34%
-

Diagnosing irritable bowel syndrome (IBS)
Relevance: 34%
-

What constitutes economic abuse under the Domestic Abuse Act 2021?
Relevance: 32%
-

How is hypotony diagnosed?
Relevance: 25%
-

How is lupus diagnosed in children?
Relevance: 25%
-

How is Chikungunya virus infection diagnosed?
Relevance: 24%
-

How is autism diagnosed?
Relevance: 24%
-

Lyme disease: What is it?
Relevance: 24%
-

How is SAD diagnosed?
Relevance: 24%
-

What is Lyme Disease?
Relevance: 24%
-

How is ADHD diagnosed?
Relevance: 24%
-
How is mitochondrial disease diagnosed?
Relevance: 24%
-

How is heart failure diagnosed?
Relevance: 24%
-

How is gonorrhoea diagnosed?
Relevance: 24%
-

How is Rubella diagnosed?
Relevance: 23%
-

Who is at risk of developing Crohn's disease?
Relevance: 23%
-

How is Super Flu diagnosed?
Relevance: 23%
-

Can children develop Crohn's disease?
Relevance: 23%
-
What is Parkinson's disease?
Relevance: 23%
-

How can eczema be diagnosed?
Relevance: 23%
-

How is psoriasis diagnosed?
Relevance: 23%
-

How is shingles diagnosed?
Relevance: 22%
Diagnosing Coeliac Disease Updated 2021
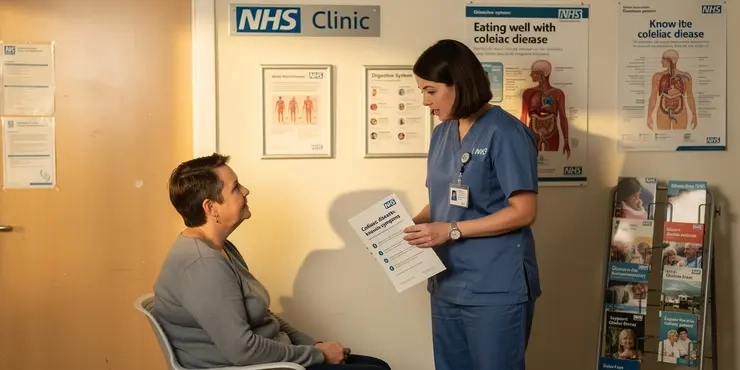
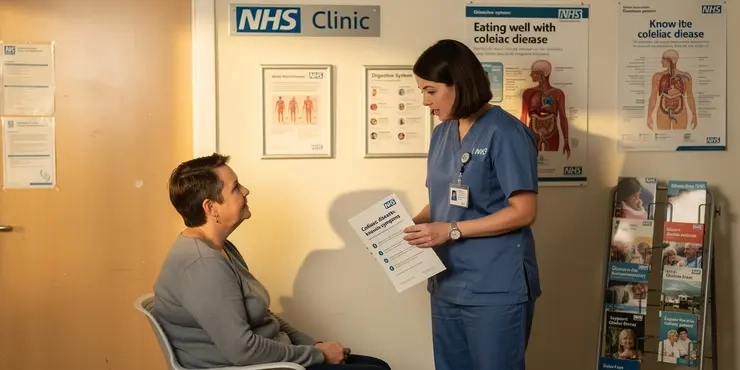
Understanding Coeliac Disease
Coeliac disease is an autoimmune disorder where the ingestion of gluten leads to damage in the small intestine. It affects approximately 1 in 100 people in the UK, although many remain undiagnosed. The only current treatment is a strict, lifelong gluten-free diet.
Recognising Symptoms
Symptoms of coeliac disease can vary widely among individuals and can affect any area of the body. Common symptoms include gastrointestinal problems such as diarrhoea, abdominal pain, and bloating. Non-gastrointestinal symptoms may include fatigue, anaemia, osteoporosis, and skin rashes. Because of this variability, coeliac disease can often be misdiagnosed or remain undiagnosed for years.
Initial Screening: Blood Tests
The first step in diagnosing coeliac disease typically involves blood tests that check for specific antibodies. The most common tests include:
- Tissue transglutaminase antibodies (tTG-IgA)
- Endomysial antibodies (EMA-IgA)
- Deamidated gliadin peptide antibodies (DGP-IgA and DGP-IgG)
It's important to note that patients should continue consuming gluten while these tests are conducted to avoid false-negative results. If these blood tests suggest coeliac disease, further diagnostic steps are recommended.
Confirmatory Diagnosis: Biopsy
If initial blood tests are positive, the next step is typically an endoscopic biopsy of the small intestine, conducted by a gastroenterologist. During this procedure, small tissue samples are taken from the lining of the small intestine to look for damage to the villi, which are the small, finger-like projections that absorb nutrients. If villous atrophy is observed, a diagnosis of coeliac disease is confirmed.
Genetic Testing
Genetic testing for HLA-DQ2 and HLA-DQ8 genes can support the diagnosis, although it is not definitive, as these genes are present in about 30% of the UK population. However, a negative result for these genes can effectively exclude coeliac disease as a diagnosis.
Post-Diagnosis: Management and Follow-Up
Once diagnosed, patients must adhere to a strict gluten-free diet, eliminating all sources of wheat, barley, and rye. Follow-up care is crucial to monitor the patient’s response to the diet, usually involving periodic blood tests to check for nutrient deficiencies and whether the coeliac-specific antibodies have returned to normal levels.
Conclusion
Early and accurate diagnosis of coeliac disease is essential to prevent long-term health complications. If you suspect you have coeliac disease, consult your GP who can guide you through the necessary diagnostic procedures. Awareness and understanding of coeliac disease have significantly improved in the UK, contributing to better patient outcomes.
Diagnosing Coeliac Disease Updated 2021
What is Coeliac Disease?
Coeliac disease is a health problem. When people with it eat gluten, it harms their small intestine. About 1 in 100 people in the UK have it, but many do not know. The only treatment is to always eat food without gluten.
How to Spot Symptoms
Symptoms can be different for everyone. Some symptoms are stomach problems like diarrhoea, tummy ache, and feeling bloated. Other symptoms can be feeling very tired, having weak bones, and skin rashes. Because symptoms can vary, it's easy to miss or get the wrong diagnosis.
First Test: Blood Tests
The first step to find out if someone has coeliac disease is usually a blood test. This test looks for certain antibodies. The main tests are:
- Tissue transglutaminase antibodies (tTG-IgA)
- Endomysial antibodies (EMA-IgA)
- Deamidated gliadin peptide antibodies (DGP-IgA and DGP-IgG)
It's important to keep eating gluten before the test to get the right result. If the blood tests show signs of coeliac disease, more tests are needed.
Next Step: Biopsy
If blood tests are positive, the next step is usually a biopsy of the small intestine. A doctor called a gastroenterologist does this test. They take tiny pieces of the intestine to see if it is damaged. If they see damage, the person has coeliac disease.
Genetic Tests
Genetic tests can help, but they don't give a definite answer because 30% of people in the UK have these genes. However, if the test is negative, it usually means the person does not have coeliac disease.
After Diagnosis: Diet and Check-Ups
After doctor says someone has coeliac disease, they must not eat any gluten. This means no wheat, barley, or rye. Regular check-ups are important. Doctors will do more blood tests to see if they are healthy and if their body is getting better.
Conclusion
It's important to find out early if someone has coeliac disease. This helps to avoid other health problems. If you think you have coeliac disease, talk to your doctor for the right tests. More people in the UK now understand coeliac disease, which helps patients get better care.
Frequently Asked Questions
What is coeliac disease?
Coeliac disease is an autoimmune disorder where the ingestion of gluten leads to damage in the small intestine.
What are the symptoms of coeliac disease?
Common symptoms include diarrhoea, abdominal pain, bloating, and nutritional deficiencies, among others. Some individuals may also experience joint pain and fatigue.
How is coeliac disease diagnosed?
Diagnosis typically involves blood tests to check for specific antibodies and a biopsy of the small intestine to assess any damage to the villi.
What blood tests are used to diagnose coeliac disease?
The most common blood tests are tissue transglutaminase antibodies (tTG-IgA) and endomysial antibodies (EMA).
Does a patient need to be eating gluten before testing for coeliac disease?
Yes, it is crucial to continue eating gluten-containing foods before the testing to ensure accurate results.
Can coeliac disease develop at any age?
Yes, coeliac disease can develop at any age, from infancy to adulthood.
What happens if coeliac disease is left untreated?
Untreated coeliac disease can lead to serious health complications, including osteoporosis, infertility, neurological conditions, and an increased risk of some cancers.
Is there a cure for coeliac disease?
There is no cure for coeliac disease, but it can be effectively managed with a strict, lifelong gluten-free diet.
What foods should be avoided by someone with coeliac disease?
Foods containing wheat, barley, and rye should be avoided. This includes bread, pasta, cereals, and many processed foods unless specifically labeled as gluten-free.
Can oats be included in a gluten-free diet for coeliac disease?
Pure, uncontaminated oats can be consumed by many people with coeliac disease, but they should be introduced cautiously and under medical supervision.
How long does it take to feel better after starting a gluten-free diet?
Many people start to feel better within a few weeks, but complete healing of the intestine may take several months to years.
Is coeliac disease hereditary?
Yes, coeliac disease has a genetic component, and first-degree relatives of a person with coeliac disease have a higher risk of developing the condition.
Are there any medications for coeliac disease?
Currently, there are no medications available to treat coeliac disease. The primary treatment is a strict gluten-free diet.
How can I avoid cross-contamination with gluten?
Avoid cross-contamination by using separate cooking utensils, toasters, and food storage containers. Also, ensure thorough cleaning of kitchen surfaces and hands.
Where can I find support for living with coeliac disease?
Support can be found through coeliac disease patient groups, such as Coeliac UK, which provide resources, advice, and emotional support.
What is coeliac disease?
Coeliac disease is when your body does not like gluten. Gluten is found in some foods like bread, pasta, and cakes.
When people with coeliac disease eat gluten, it can make them feel unwell. Signs might be tummy pain, feeling tired, or feeling sick.
If you think you have coeliac disease, it is important to talk to a doctor.
To support understanding, you can use pictures or find easy videos online about coeliac disease.
Coeliac disease is a health problem. It happens when the body does not like gluten. Eating gluten can hurt the small intestine.
What happens when you have coeliac disease?
Some common signs are runny poo, tummy pain, feeling full and gassy, and not getting enough important body stuff from food. Some people might also feel sore in their joints and very tired.
How do doctors find out if someone has coeliac disease?
To find out what's wrong, doctors usually do two things. First, they take some blood to look for special signs in it. Second, they take a tiny piece from inside the tummy to see if it is hurt.
If you find reading hard, try using a ruler to follow the lines. Reading slowly and taking breaks can also help.
What blood tests help find out if someone has coeliac disease?
If the doctor thinks you might have coeliac disease, they can use some special blood tests to find out. These tests look for certain things in your blood that are higher if you have coeliac disease.
Here are some tools and tips that might help:
- Ask the doctor to explain each blood test in simple words.
- Write down any questions you have before visiting the doctor.
- A family member or friend can join you to help remember what the doctor says.
The most common blood tests are called tTG-IgA and EMA. They help doctors check for certain health problems.
Do you need to eat gluten before a test for coeliac disease?
Yes, you should eat gluten before the test. Gluten is in foods like bread, pasta, and cereal.
Eating gluten helps the doctor see if your body reacts to it during the test.
If you have trouble reading or understanding this, a friend or family member can help explain it.
Using pictures or symbols can also make it easier to understand.
Yes, it is very important to keep eating foods with gluten before the test. This helps get the right test results.
Can you get coeliac disease at any age?
Yes, you can get coeliac disease at any age. Children and grown-ups can both get it.
Coeliac disease is when your body doesn't like gluten. Gluten is in things like bread and pasta.
If you don't feel well after eating these foods, talk to a doctor. A doctor can help find out if you have coeliac disease.
Using pictures or talking with someone can help make it easier to understand this.
Yes, coeliac disease can start at any age. It can happen to babies, children, or adults.
What happens if coeliac disease is not treated?
If someone with coeliac disease does not get treatment, it can make them feel very sick. Their body may not get the right nutrients from food, which can lead to feeling tired or weak.
Other problems might happen too, like stomach aches or damage to parts of the body. It's important to see a doctor and follow their advice to feel better.
People with coeliac disease can use tools like food diaries to help them keep track of what they eat. This can make it easier to manage the condition.
If you don’t treat coeliac disease, it can make you very sick. It can cause weak bones, problems having babies, brain issues, and even some kinds of cancer.
Can coeliac disease be cured?
No, coeliac disease can't be cured. But you can feel better by not eating gluten. Gluten is in bread, pasta, and cakes. Many people use special apps to check what food is safe to eat. Talking to a doctor or a dietitian can also help.
There is no cure for coeliac disease, but you can manage it by always eating gluten-free foods.
What foods should someone with coeliac disease stay away from?
People with coeliac disease cannot eat gluten. Gluten is found in some grains like wheat, barley, and rye.
Here are some foods to avoid:
- Bread made from wheat
- Pasta made from wheat
- Cookies and cakes with wheat
- Cereals with barley or rye
- Beer made from barley
It's important to read food labels carefully. Look for "gluten-free" on packages.
Support tools: It can be helpful to use a gluten-free app or a shopping list to remember which foods are safe.
Some foods have wheat, barley, and rye in them. You should not eat these foods. This means no bread, pasta, cereals, and other foods that come in packets. Look for foods with a label that says "gluten-free" to be safe.
Can people with coeliac disease eat oats?
People with coeliac disease need to avoid gluten. Gluten is found in some grains like wheat. Oats do not have gluten. But sometimes, oats are made near other grains with gluten. This can make oats unsafe for some people with coeliac disease.
If you have coeliac disease, you should look for "gluten-free oats" on the label. These are safe to eat because they are not made near grains with gluten.
If you are not sure, talk to a doctor or dietitian. They can help you know what is safe for you to eat.
Using a food diary can help you track what you eat. You can also use an app to learn more about gluten-free foods.
Many people with coeliac disease can eat oats if they are very clean and safe. But it is important to try them slowly and have a doctor help you.
How long until I feel better after stopping gluten?
When you stop eating foods with gluten, you might start to feel better. This can take some time. Some people feel better in a few days. For others, it might take a few weeks.
Here are some tips to help you:
- Be patient. Everyone is different. Your body needs time to heal.
- Keep a simple food diary. Write down what you eat and how you feel.
- Talk to a doctor if you are worried.
A lot of people start to feel better a few weeks after getting sick. But it can take a long time for the tummy to get all better. Sometimes, it can take months or even years.
If you need extra help reading, you could use a ruler to follow each line or ask someone to read with you. You can also try reading out loud. It can make the words easier to understand.
Does coeliac disease run in families?
Coeliac disease can be passed down from parents to children. This means if someone in your family has it, you might have it too.
Here are some things that can help:
- Talk to your doctor if someone in your family has coeliac disease.
- They might suggest a test to see if you have it.
- Eating the right foods can help you feel better if you have coeliac disease.
Yes, coeliac disease can run in families. If someone in your family, like a parent or sibling, has coeliac disease, you are more likely to get it too.
If you find this hard to read, you can try using a ruler or your finger to follow the words. You can also ask someone to read it to you.
Is there medicine for coeliac disease?
There are no medicines to help people with coeliac disease right now. The main way to feel better is to eat food without gluten.
How can I keep away from gluten mixing with my food?
Here are some tips:
- Use different tools: Have separate knives, forks, and spoons just for gluten-free food.
- Clean surfaces: Wipe down tables and counters before making gluten-free meals.
- Use separate toasters: Have a different toaster for gluten-free bread.
- Label foods: Put labels on containers to show which are gluten-free.
- Store foods apart: Keep gluten-free and gluten foods in different places.
If you need help, you can also ask someone to show you or use pictures to remind you.
Keep food safe. Use different cooking tools, toasters, and containers for each type of food. Always clean the kitchen surfaces and wash your hands well.
Where can I get help if I have coeliac disease?
Coeliac disease is when you get sick from eating gluten. Gluten is in foods like bread and pasta.
If you have coeliac disease, you can get help by:
- Talking to a doctor: A doctor can tell you what foods to eat and avoid.
- Joining a support group: You can meet other people with the same condition. They can share tips and advice.
- Finding information online: Websites have lots of information about coeliac disease.
- Asking a dietitian: A dietitian can help you plan meals that are safe to eat.
Remember to always ask for help if you need it. It's important to stay healthy and feel good.
You can get help from groups for people with coeliac disease, like Coeliac UK. They give you useful information, advice, and can make you feel better.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Diagnosing Coeliac Disease Updated 2021
Relevance: 100%
-

Coeliac Disease: Session 1: What is Coeliac Disease?
Relevance: 71%
-

Coeliac disease
Relevance: 71%
-

NHSGGC - What is Coeliac Disease?
Relevance: 65%
-

Causes of coeliac disease
Relevance: 65%
-

Symptoms of coeliac disease
Relevance: 62%
-

Coeliac Disease: The gluten free diet
Relevance: 62%
-

Living Well with Coeliac Disease
Relevance: 61%
-
Coeliac Disease Explained - Gluten Sensitivity - A to Z of the NHS - Dr Gill
Relevance: 54%
-

How is Crohn's disease diagnosed?
Relevance: 38%
-

Diverticular Nov 2021
Relevance: 38%
-

How is Huntington's disease diagnosed?
Relevance: 38%
-

How is Alzheimer's disease diagnosed?
Relevance: 37%
-

How is flesh-eating disease diagnosed?
Relevance: 37%
-

When did the Domestic Abuse Act 2021 come into effect?
Relevance: 36%
-

How is sickle cell disease diagnosed?
Relevance: 36%
-

What tests are available for diagnosing Lyme disease?
Relevance: 35%
-

How is Marburg virus disease diagnosed?
Relevance: 35%
-

How is motor neurone disease diagnosed?
Relevance: 34%
-

Diagnosing irritable bowel syndrome (IBS)
Relevance: 34%
-

What constitutes economic abuse under the Domestic Abuse Act 2021?
Relevance: 32%
-

How is hypotony diagnosed?
Relevance: 25%
-

How is lupus diagnosed in children?
Relevance: 25%
-

How is Chikungunya virus infection diagnosed?
Relevance: 24%
-

How is autism diagnosed?
Relevance: 24%
-

Lyme disease: What is it?
Relevance: 24%
-

How is SAD diagnosed?
Relevance: 24%
-

What is Lyme Disease?
Relevance: 24%
-

How is ADHD diagnosed?
Relevance: 24%
-
How is mitochondrial disease diagnosed?
Relevance: 24%
-

How is heart failure diagnosed?
Relevance: 24%
-

How is gonorrhoea diagnosed?
Relevance: 24%
-

How is Rubella diagnosed?
Relevance: 23%
-

Who is at risk of developing Crohn's disease?
Relevance: 23%
-

How is Super Flu diagnosed?
Relevance: 23%
-

Can children develop Crohn's disease?
Relevance: 23%
-
What is Parkinson's disease?
Relevance: 23%
-

How can eczema be diagnosed?
Relevance: 23%
-

How is psoriasis diagnosed?
Relevance: 23%
-

How is shingles diagnosed?
Relevance: 22%