
Find Help
More Items From Ergsy search
-

Is hypotony a medical emergency?
Relevance: 100%
-

Do certain medications contribute to hypotony?
Relevance: 64%
-

What is the eye condition hypotony?
Relevance: 54%
-

Can hypotony be prevented?
Relevance: 52%
-

What is hypotony in the eye?
Relevance: 52%
-

How common is hypotony?
Relevance: 52%
-

What causes hypotony?
Relevance: 51%
-

What should I do if I suspect I have hypotony?
Relevance: 50%
-

What treatments are available for hypotony?
Relevance: 50%
-

Can hypotony affect vision?
Relevance: 50%
-

What are the symptoms of hypotony?
Relevance: 49%
-

How is hypotony diagnosed?
Relevance: 49%
-

Can hypotony occur in both eyes?
Relevance: 48%
-

Are there any risk factors for developing hypotony?
Relevance: 48%
-

Can hypotony recur after treatment?
Relevance: 48%
-

Can hypotony resolve on its own?
Relevance: 48%
-

What is the difference between hypotony and glaucoma?
Relevance: 46%
-

Why is meningitis a medical emergency?
Relevance: 46%
-

Can wearing contact lenses affect hypotony?
Relevance: 44%
-

Are there any lifestyle changes that can help with hypotony?
Relevance: 44%
-

What complications can arise from untreated hypotony?
Relevance: 44%
-

What should I do in case of a medical emergency while in the EU?
Relevance: 43%
-

How are emergencies handled in a virtual ward?
Relevance: 35%
-

How do live-in caregivers handle emergencies?
Relevance: 35%
-
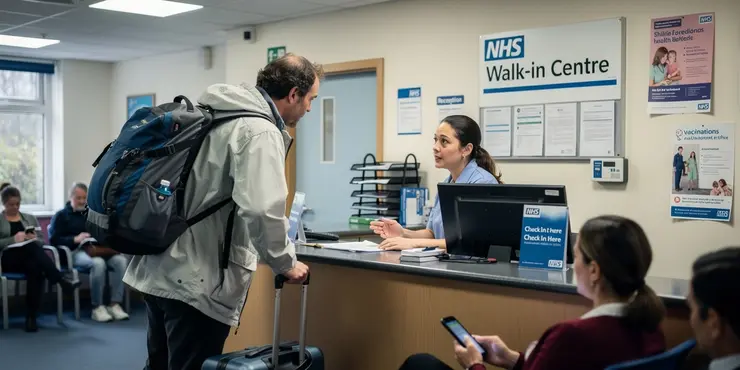
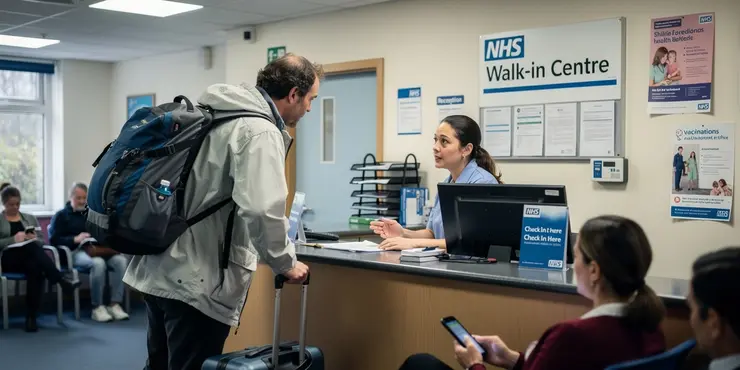
What if I need emergency assistance while traveling?
Relevance: 33%
-

How can community helpers access emergency assistance?
Relevance: 32%
-

Can I get an emergency NHS dental appointment?
Relevance: 31%
-
Are new emerging pathogens a risk for blood safety?
Relevance: 30%
-
Do I need to be a registered patient to get emergency NHS dental care?
Relevance: 28%
-
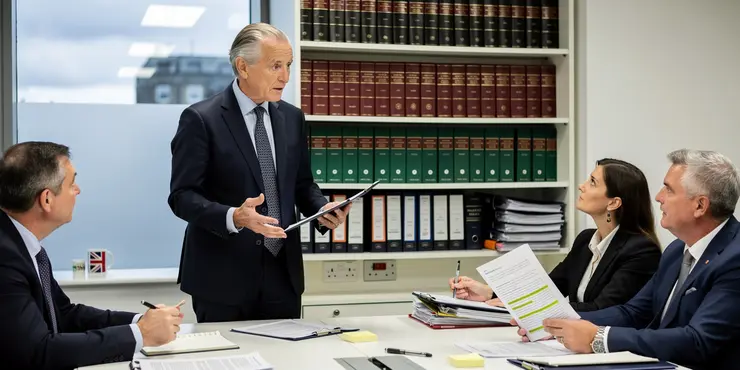
Public Inquiry into States of Emergency: Legal Experts Demand Transparency
Relevance: 28%
-
How often do new COVID-19 variants emerge?
Relevance: 27%
-

Is medical treatment covered by insurance when traveling to the EU?
Relevance: 26%
-

What are the medical uses of ketamine?
Relevance: 25%
-

Are there any new mosquito-borne diseases emerging in the UK in 2025?
Relevance: 25%
-

Do care homes provide medical care?
Relevance: 24%
-

Is it possible to travel with a medical escort to an EU country?
Relevance: 23%
-

Do I need a referral to receive medical treatment in the EU?
Relevance: 22%
-
Can I travel to EU countries for medical treatment?
Relevance: 21%
-

Can I travel to EU countries for medical treatment?
Relevance: 21%
-

Are GLP-1 medications injectable?
Relevance: 21%
Is Hypotony a Medical Emergency?
Hypotony refers to abnormally low intraocular pressure (IOP) in the eye, typically considered as pressure less than 6 mmHg. While not as commonly discussed as high intraocular pressure, which is often associated with conditions like glaucoma, hypotony can have significant implications for ocular health and function.
In the UK, as in many parts of the world, the management of hypotony depends on its underlying cause and the presence of any complications. It is essential to determine whether hypotony is indeed a medical emergency, as this affects how quickly and aggressively it needs to be treated.
Causes of hypotony vary and can include surgical complications, ocular trauma, inflammation within the eye (such as uveitis), retinal detachment, or cyclodialysis clefts. Certain conditions, such as over-filtration after glaucoma surgery, might also lead to this state. The seriousness of hypotony largely depends on its duration, underlying cause, and the presence of symptoms or complications.
Acute hypotony, especially if it arises suddenly after an eye surgery or trauma, is often considered more of an emergency. This scenario demands immediate medical evaluation as it can lead to potentially rapid progression to visual impairment. Left untreated, chronic hypotony can result in structural changes in the eye, such as choroidal detachment or maculopathy, which can lead to permanent vision loss.
Symptoms often associated with hypotony include visual disturbances like blurriness, double vision, and field loss. Physical signs may include a shallow anterior chamber or collapsed eye wall. These symptoms suggest that prompt ophthalmologic assessment is important to prevent irreversible damage.
Treatment for hypotony in the UK typically focuses on addressing the underlying cause. For instance, if a surgical site is leaking, surgical repair may be warranted to restore normal intraocular pressure. Medical treatment could involve corticosteroids or other medications to reduce inflammation, or adjustments in medications if the hypotony is drug-induced.
In an emergency setting, or if vision-threatening complications have occurred, an urgent referral to an ophthalmologist is necessary. Here, the expert will evaluate the specific condition of the eye and decide on the most appropriate corrective action.
In summary, while hypotony itself may not always be an outright emergency, its potential consequences necessitate timely professional evaluation and intervention. Proper diagnosis and treatment are crucial to prevent long-term damage and maintain eye health. If you suspect hypotony or experience any related symptoms, contacting a healthcare professional without delay is advised to ensure prompt care.
Frequently Asked Questions
What is hypotony?
Hypotony refers to abnormally low intraocular pressure in the eye, often leading to vision problems or other complications.
Is hypotony considered a medical emergency?
Hypotony can be a medical emergency if it leads to vision loss or other serious complications. Immediate medical attention is often necessary.
What are the symptoms of hypotony?
Symptoms of hypotony include blurry vision, visual disturbances, eye discomfort, and on examination, a soft eye on palpation.
What causes hypotony?
Hypotony can be caused by surgical complications, trauma, inflammation, retinal detachment, or certain eye diseases.
How is hypotony diagnosed?
Hypotony is diagnosed by measuring the intraocular pressure, typically using tonometry, and by assessing symptoms and eye health.
What is the normal range for intraocular pressure?
The normal range for intraocular pressure is usually between 10 and 21 mmHg. Hypotony is often defined as pressure below 6 mmHg.
Can hypotony cause permanent vision loss?
Yes, if left untreated, hypotony can lead to permanent vision loss due to structural damage to the eye or retinal problems.
What treatments are available for hypotony?
Treatment options for hypotony include medical management, surgical intervention, or addressing underlying causes like inflammation.
How quickly should hypotony be treated?
Hypotony should be addressed as soon as possible, especially if there is a risk of vision loss or other complications.
What are potential complications of untreated hypotony?
Complications of untreated hypotony can include choroidal detachment, retinal detachment, cataracts, or permanent visual impairment.
Is low intraocular pressure always a cause for concern?
While low pressure can sometimes be benign, significantly low pressure can be concerning and should be evaluated by an eye specialist.
Can hypotony occur in both eyes?
Yes, hypotony can occur in one or both eyes, though it more commonly affects one eye due to localized issues.
Should I see an ophthalmologist if I suspect hypotony?
Yes, seeing an ophthalmologist promptly is crucial if hypotony is suspected, as they can assess and manage the condition appropriately.
What surgical procedures can lead to hypotony?
Procedures such as glaucoma surgery or retinal surgery can sometimes lead to hypotony as a complication.
Can medications cause hypotony?
Certain medications used for treating eye conditions can potentially lead to hypotony as a side effect.
How do eye doctors measure intraocular pressure?
Intraocular pressure is commonly measured using tonometry, which involves applying a small amount of pressure to the eye.
Can hypotony occur after eye trauma?
Yes, eye trauma is a known cause of hypotony, especially if it disrupts the eye's structure or intraocular contents.
Is hypotony more common in certain populations?
Hypotony can occur in any population but may be more common in those undergoing surgeries for glaucoma or retinal conditions.
Are there preventive measures for hypotony?
Preventive measures include careful management of eye surgeries, controlling uveitis, and closely monitoring patients at risk.
How does hypotony affect vision?
Hypotony can affect vision by causing retinal changes, folds in the choroid, or by leading to other ocular structural changes.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Is hypotony a medical emergency?
Relevance: 100%
-

Do certain medications contribute to hypotony?
Relevance: 64%
-

What is the eye condition hypotony?
Relevance: 54%
-

Can hypotony be prevented?
Relevance: 52%
-

What is hypotony in the eye?
Relevance: 52%
-

How common is hypotony?
Relevance: 52%
-

What causes hypotony?
Relevance: 51%
-

What should I do if I suspect I have hypotony?
Relevance: 50%
-

What treatments are available for hypotony?
Relevance: 50%
-

Can hypotony affect vision?
Relevance: 50%
-

What are the symptoms of hypotony?
Relevance: 49%
-

How is hypotony diagnosed?
Relevance: 49%
-

Can hypotony occur in both eyes?
Relevance: 48%
-

Are there any risk factors for developing hypotony?
Relevance: 48%
-

Can hypotony recur after treatment?
Relevance: 48%
-

Can hypotony resolve on its own?
Relevance: 48%
-

What is the difference between hypotony and glaucoma?
Relevance: 46%
-

Why is meningitis a medical emergency?
Relevance: 46%
-

Can wearing contact lenses affect hypotony?
Relevance: 44%
-

Are there any lifestyle changes that can help with hypotony?
Relevance: 44%
-

What complications can arise from untreated hypotony?
Relevance: 44%
-

What should I do in case of a medical emergency while in the EU?
Relevance: 43%
-

How are emergencies handled in a virtual ward?
Relevance: 35%
-

How do live-in caregivers handle emergencies?
Relevance: 35%
-
What if I need emergency assistance while traveling?
Relevance: 33%
-

How can community helpers access emergency assistance?
Relevance: 32%
-

Can I get an emergency NHS dental appointment?
Relevance: 31%
-
Are new emerging pathogens a risk for blood safety?
Relevance: 30%
-
Do I need to be a registered patient to get emergency NHS dental care?
Relevance: 28%
-
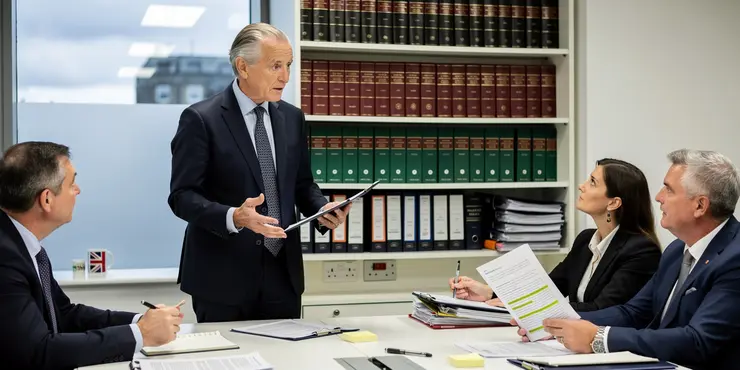
Public Inquiry into States of Emergency: Legal Experts Demand Transparency
Relevance: 28%
-
How often do new COVID-19 variants emerge?
Relevance: 27%
-

Is medical treatment covered by insurance when traveling to the EU?
Relevance: 26%
-

What are the medical uses of ketamine?
Relevance: 25%
-

Are there any new mosquito-borne diseases emerging in the UK in 2025?
Relevance: 25%
-

Do care homes provide medical care?
Relevance: 24%
-

Is it possible to travel with a medical escort to an EU country?
Relevance: 23%
-

Do I need a referral to receive medical treatment in the EU?
Relevance: 22%
-
Can I travel to EU countries for medical treatment?
Relevance: 21%
-

Can I travel to EU countries for medical treatment?
Relevance: 21%
-

Are GLP-1 medications injectable?
Relevance: 21%


