Find Help
More Items From Ergsy search
-

Physiotherapy Assessment of Urinary Incontinence
Relevance: 100%
-

Avoiding infections with urinary incontinence
Relevance: 60%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 58%
-

Pelvic health: stress urinary incontinence
Relevance: 56%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 55%
-

Newcastle Specialist Continence Service's Light Urinary Incontinence Project
Relevance: 53%
-
Incontinence | NHS
Relevance: 46%
-
Pelvic health: Urge Incontinence
Relevance: 39%
-

Is a prescription needed for air physiotherapy?
Relevance: 28%
-

What is air physiotherapy?
Relevance: 27%
-

What qualifications should a provider of air physiotherapy have?
Relevance: 27%
-

Sandwell and West Birmingham Hospitals NHS Trust – Faecal Incontinence and Constipation Healthcare
Relevance: 26%
-

What equipment is used in air physiotherapy?
Relevance: 26%
-

Can air physiotherapy be done at home?
Relevance: 26%
-

How does air physiotherapy work?
Relevance: 26%
-
Are there any exercises involved in air physiotherapy?
Relevance: 26%
-
Your pelvic health matters: insights from NHS clinicians
Relevance: 25%
-

Does air physiotherapy involve medication?
Relevance: 25%
-

NHSGGC - Respiratory Physiotherapy Service: Self-Management
Relevance: 25%
-
Who can benefit from air physiotherapy?
Relevance: 24%
-

Can air physiotherapy prevent respiratory infections?
Relevance: 24%
-

The Leeds Specialist Rehabilitation Centre - 3 Prosthetic Physiotherapy
Relevance: 24%
-
Can air physiotherapy help with COVID-19 recovery?
Relevance: 23%
-

How often should one perform air physiotherapy?
Relevance: 23%
-

Physiotherapy Exercises following an Ankle Fracture
Relevance: 23%
-

Part One: Understanding Osteoarthritis- MSK Physiotherapy
Relevance: 22%
-

How does surgery treat prostate cancer?
Relevance: 19%
-

How is PIP assessed?
Relevance: 19%
-

What is an incentive spirometer in air physiotherapy?
Relevance: 18%
-

How do I register for Self Assessment?
Relevance: 18%
-

What are the side effects of prostate cancer surgery?
Relevance: 18%
-

Who is responsible for assessing SEND needs?
Relevance: 17%
-

What is a Self Assessment tax return?
Relevance: 17%
-

Social Services and Well-being (Wales) Act: Assessments
Relevance: 16%
-

My first Self Assessment tax return
Relevance: 16%
-
Autism Assessment - What Happens in Your Appointment
Relevance: 16%
-

How do I complete my Self Assessment tax return?
Relevance: 16%
-

What is the role of mental health assessments in indefinite sentences?
Relevance: 16%
-

Are there any complications associated with untreated BPH?
Relevance: 16%
-

Can I get help from HMRC with my Self Assessment?
Relevance: 16%
Physiotherapy Assessment of Urinary Incontinence
Introduction to Urinary Incontinence
Urinary incontinence is a common condition affecting many individuals in the United Kingdom, particularly women and the elderly. It can significantly impact an individual’s quality of life, leading to emotional distress and social embarrassment. Physiotherapy plays a crucial role in the assessment and management of urinary incontinence, providing non-invasive treatment options to improve bladder control and pelvic floor strength.
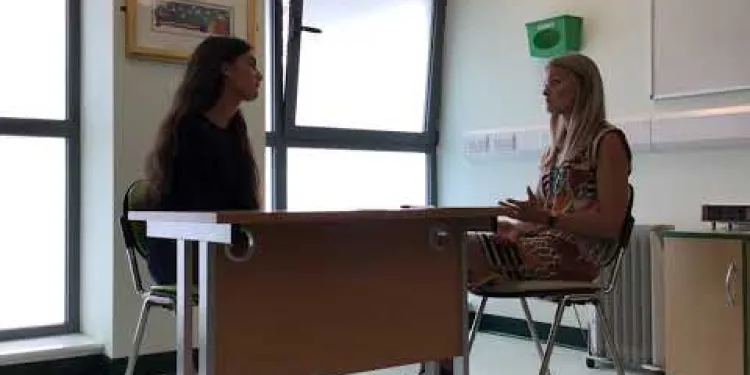
Initial Consultation and History Taking
An essential part of the physiotherapy assessment involves a thorough initial consultation. During this first session, the physiotherapist will take a detailed history of the patient’s symptoms, lifestyle, and medical background. Key information gathered includes the frequency and severity of leakage, triggers, and any existing medical conditions that may contribute to urinary incontinence. Understanding these aspects is important for crafting a personalised treatment plan.
Physical Examination
Following the initial consultation, a physical examination is conducted. This typically includes an assessment of the pelvic floor muscles, which are crucial in maintaining continence. The pelvic floor examination may involve both external and internal palpations to gauge muscle strength, endurance, and any points of tenderness. The physiotherapist may also assess abdominal muscles and posture to determine their role in the patient’s condition.
Use of Diagnostic Tools
Various diagnostic tools may be utilised to complement the physical examination. These can include ultrasound imaging to visualise the bladder, urinalysis to check for infections, and bladder diaries where patients record their fluid intake and urinary habits over a period of time. Additionally, electromyography (EMG) may be conducted to evaluate the electrical activity of pelvic floor muscles.
Developing a Treatment Plan
Based on the assessment findings, a comprehensive treatment plan is formulated. This typically involves pelvic floor muscle training (PFMT), which includes exercises to strengthen the muscles responsible for bladder control. Biofeedback and electrical stimulation may also be used to enhance muscle function. Lifestyle and dietary modifications are often recommended to support continence. Regular follow-ups are scheduled to monitor progress and adjust the treatment plan as necessary.
Conclusion
Physiotherapy offers a valuable, non-surgical approach to managing urinary incontinence. By undertaking a detailed assessment, physiotherapists can identify the underlying causes and tailor treatment to meet individual needs. This holistic approach not only improves physical function but also enhances overall well-being, helping individuals in the UK regain confidence and improve their quality of life.
Physiotherapy Check for Bladder Problems
What is Urinary Incontinence?
Urinary incontinence means having trouble controlling urine flow. It is common in many people in the UK, especially women and older adults. It can make people feel upset and embarrassed. Physiotherapy helps by using exercises and treatments that do not need surgery. These help you control your bladder better and make the muscles in your pelvis stronger.
First Meeting and Questions
The physiotherapist will start by having an important first meeting with you. They will ask many questions about your symptoms, daily activities, and any past health issues. They need to know how often accidents happen and what might cause them. Knowing these things helps them make a plan that fits you.
Physical Check-Up
After asking questions, the physiotherapist will do a physical check-up. They will look at the muscles that help you hold urine. This can include checking from the outside and sometimes a gentle check from inside to see how strong the muscles are. They might also look at your tummy muscles and how you stand because these can affect your bladder control.
Special Tests
Sometimes, special tests are used to understand more. These can include using an ultrasound to see the bladder, checking urine for infections, and keeping a diary of when you drink and use the toilet. Another test might be checking how the muscles work using a tool that measures electrical signals in muscles (EMG).
Making a Treatment Plan
After all the checks, the physiotherapist will make a plan just for you. This usually includes exercises to make your pelvic muscles stronger. They might use special devices to show how your muscles are working. Changes in what you eat and drink might also help. You will have regular meetings to see how you are doing and change the plan if needed.
Summary
Physiotherapy is a helpful and gentle way to manage bladder control problems without surgery. A careful check-up helps find what causes the trouble, and the physiotherapist makes a special plan for you. By improving your muscle strength and habits, you can feel better, gain confidence, and enjoy life more.
Frequently Asked Questions
What is urinary incontinence?
Urinary incontinence is the unintentional loss of bladder control, leading to the leakage of urine.
Who can get urinary incontinence?
Urinary incontinence can affect people of all ages, but it is more common in older adults and women.
What are the types of urinary incontinence?
The main types include stress incontinence, urge incontinence, overflow incontinence, and functional incontinence.
What causes urinary incontinence?
Common causes include pregnancy, childbirth, menopause, obesity, pelvic floor disorders, and certain medical conditions.
How is urinary incontinence diagnosed?
Diagnosis involves a physical exam, patient history, bladder diary, and potentially urodynamic tests or imaging.
What is a physiotherapy assessment for urinary incontinence?
A physiotherapy assessment involves evaluating pelvic floor muscle function, bladder habits, and lifestyle factors contributing to incontinence.
What will happen during a physiotherapy assessment for urinary incontinence?
The physiotherapist will review your medical history, conduct a physical examination, and assess your pelvic floor muscles and bladder habits.
How long does a physiotherapy assessment for urinary incontinence take?
An initial assessment typically lasts about 45 to 60 minutes.
What treatments can a physiotherapist offer for urinary incontinence?
Treatments include pelvic floor exercises, bladder training, lifestyle advice, and sometimes biofeedback or electrical stimulation.
Are pelvic floor exercises effective?
Yes, consistent pelvic floor exercises can significantly improve symptoms of urinary incontinence.
Can men benefit from physiotherapy for urinary incontinence?
Yes, men can also benefit from pelvic floor exercises and other physiotherapy treatments, especially after prostate surgery.
Is urinary incontinence preventable?
While not all cases are preventable, maintaining a healthy weight, doing regular pelvic floor exercises, and avoiding bladder irritants can reduce risk.
Will I need to see a physiotherapist regularly?
Frequency of visits depends on individual progress, but follow-ups are usually recommended to monitor improvement and adjust treatment.
Can urinary incontinence be cured?
Many cases of urinary incontinence can be significantly improved or cured with proper treatment, though results vary by individual.
What should I wear to a physiotherapy appointment for urinary incontinence?
Wear comfortable clothing that allows easy access to your abdomen and pelvic area for examination purposes.
What is urinary incontinence?
Urinary incontinence means you might pee when you don't want to. It can be hard to stop pee from coming out. Here are some ways to help:
- Do special exercises to make your pee muscles strong. These are called Kegel exercises.
- Visit a doctor or nurse for help.
- Use products like special pads to stay dry.
- Ask someone you trust to support you.
Urinary incontinence is when you cannot control your bladder and accidentally pee.
Who can have trouble holding pee?
Having trouble controlling your bladder can happen to anyone. But it happens more to older people and women.
What kinds of urinary incontinence are there?
Urinary incontinence means having trouble controlling your bladder. Here are some types:
Stress incontinence: Leaking pee when you laugh, sneeze, or lift something heavy.
Urge incontinence: Feeling a strong need to pee and not being able to reach the toilet in time.
Overflow incontinence: Not being able to empty your bladder all the way, so some pee dribbles out later.
Functional incontinence: Having trouble moving, thinking, or communicating, which makes it hard to get to the toilet in time.
Tip: Using a bathroom schedule and wearing special pads can help manage incontinence. Ask a doctor for more advice.
There are different types of incontinence. They are:
- Stress incontinence: This happens when you leak pee because of sneezing, coughing, or laughing.
- Urge incontinence: This is when you suddenly need to pee and can't hold it in.
- Overflow incontinence: This is when your bladder doesn't empty properly and you leak pee.
- Functional incontinence: This happens if something makes it hard to reach the bathroom in time.
If you have trouble reading, try using tools like audiobooks or text-to-speech apps. They can read the text out loud for you. Also, breaking information into small parts or using pictures can help you understand better.
Why do some people have trouble holding their pee?
There are many reasons why this can happen. It can happen if you are having a baby, just had a baby, or are older. Being very overweight can make it happen too. It can also happen if the muscles in your lower belly are weak or if you have certain health problems.
How do doctors find out if someone has trouble holding pee?
The doctor will check your body and ask about your health. They might ask you to write down when you pee in a bladder diary. They might also do some special tests or use pictures to look inside your body.
What Happens at a Physiotherapy Check for Bladder Leaks?
If you leak pee sometimes, a physiotherapist can help. This is called a bladder leak check.
First, the physiotherapist will ask you some questions. They want to know when and how often you leak. They may ask about your health and what you eat and drink.
Next, the physiotherapist might do some simple tests. These tests help them understand how strong your muscles are.
To help you feel better, the physiotherapist will show you exercises. These exercises make your muscles stronger so you can hold your pee better.
If you want help, there are ways to make it easier:
- Bring a family member or friend with you to the appointment.
- Ask questions if you don't understand something.
- Write down what the physiotherapist says so you can remember later.
A physiotherapy check-up helps find out how your pelvic floor muscles work. It also looks at how often you use the bathroom and parts of your lifestyle that might cause leaks.
Tools that might help include reminders to go to the bathroom or simple exercises for stronger muscles.
What will happen during a physiotherapy check-up for bladder problems?
When you visit a physiotherapist for bladder problems, they will do a check-up to see how they can help you. Here’s what usually happens:
- Talking: The physio will talk to you about your bladder problem. They will ask questions like when it happens or how often.
- Physical Check: They might look at how your muscles work. This helps them understand what's happening.
- Exercises: The physio might show you some simple exercises that can help your bladder get stronger.
- Tools to Help: Some people use apps or reminders to remember to do their exercises. You might find these helpful too.
Remember, it's okay to ask questions if you don’t understand. The physio is there to help you feel better.
The physiotherapist will look at your health history, check your body, and see how your pelvic floor muscles and bladder work.
How long will a physiotherapy check-up for bladder issues take?
A physiotherapy check-up for bladder issues might last about 45 minutes to 1 hour.
During this time, a physiotherapist will talk to you and may do some simple tests to understand your problem.
If you find reading hard, you can ask someone to help you understand this information. You might also use audio tools or apps that read text out loud.
An initial check-up usually takes about 45 to 60 minutes.
How can a physiotherapist help if you have trouble holding pee?
A physiotherapist is someone who helps people move and feel better. If it’s hard for you to hold pee, a physiotherapist can help. They can show you exercises to make your muscles stronger. These exercises can help you hold your pee better. Using things like a picture guide for exercises can make it easier. Bullet points help you understand steps one by one. Remember, it’s okay to ask questions and take your time learning.Here are ways to help:
- Do special exercises to make your tummy muscles stronger.
- Train your bladder by going to the toilet at regular times.
- Get advice on things you can change in your life to help.
- Sometimes, doctors use special tools to help your muscles work better.
Do pelvic floor exercises help?
Yes, pelvic floor exercises can help make the muscles in your lower tummy stronger. This is good for stopping leaks when you laugh, cough, or sneeze.
If you want to try doing these exercises, it can be helpful to:
- Watch a video that shows you how to do them.
- Ask a friend or a family member to exercise with you.
- Use a reminder or alarm to help you remember to do the exercises every day.
Yes, doing pelvic floor exercises regularly can make pee leaks much better.
Can men get better with physiotherapy for bladder problems?
Sometimes men have trouble controlling their bladder, which means they might leak urine.
Physiotherapy can help with these bladder problems.
What is physiotherapy?
Physiotherapy is a way to make your muscles stronger and help your body work better.
How can it help?
- It teaches men how to do special exercises to make bladder muscles strong.
- These exercises can stop or reduce leaking.
If you're having problems, it's a good idea to see a doctor or physiotherapist. They can help you find the right exercises.
You might find it useful to use reminders to practice exercises and ask someone you trust for support.
Yes, men can do pelvic floor exercises too. These exercises can help a lot, especially after having surgery on their prostate.
Can we stop pee leaks from happening?
Some problems can't be stopped, but you can do some things to help. Keep a healthy weight. Do exercises to make your tummy and bladder strong. Stay away from food and drinks that bother your bladder.
Will I need to see a physiotherapist often?
If you have hurt yourself, a physiotherapist can help you get better. They are like a special doctor for your body. You might need to see them more than once. They will help you by showing you exercises. It is like training for your body.
If you need help, you can use pictures to understand better. You can also ask someone to go with you to the appointments.
How often you go back depends on how well you are doing. Doctors like to check if you are getting better and might change how they help you.
Can pee leaks be fixed?
Sometimes, people have trouble holding their pee. This is called pee leaks.
There are ways to help or fix pee leaks. Here are some ideas:
- See a doctor. They can help find the best way to fix it.
- Do special exercises, like Kegel exercises. They make the pee muscles stronger.
- Bladder training. This helps you go to the bathroom at the right times.
- Use special pads or pants if needed.
Getting some help can make pee leaks better or even go away. If you have pee leaks, talk to someone who can help, like a doctor.
You can often make wetting accidents much better or even stop them with the right help. But it works differently for each person.
What Clothes Should I Wear to See the Physio for Bladder Problems?
When you go to the physio to help with bladder problems, wear clothes that are easy to move in.
Here are some tips:
- Choose comfy clothes, like a t-shirt and loose pants or shorts.
- Wear clean underwear.
- If you have questions, ask the physio before your visit.
You can bring someone with you if it helps you feel better. It's okay to ask for help if you need it.
Wear comfy clothes. They should let the doctor easily check your tummy and hip area.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Physiotherapy Assessment of Urinary Incontinence
Relevance: 100%
-

Avoiding infections with urinary incontinence
Relevance: 60%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 58%
-

Pelvic health: stress urinary incontinence
Relevance: 56%
-

Incontinence and Prolapse - Physiotherapy Advice
Relevance: 55%
-

Newcastle Specialist Continence Service's Light Urinary Incontinence Project
Relevance: 53%
-
Incontinence | NHS
Relevance: 46%
-
Pelvic health: Urge Incontinence
Relevance: 39%
-

Is a prescription needed for air physiotherapy?
Relevance: 28%
-

What is air physiotherapy?
Relevance: 27%
-

What qualifications should a provider of air physiotherapy have?
Relevance: 27%
-

Sandwell and West Birmingham Hospitals NHS Trust – Faecal Incontinence and Constipation Healthcare
Relevance: 26%
-

What equipment is used in air physiotherapy?
Relevance: 26%
-

Can air physiotherapy be done at home?
Relevance: 26%
-

How does air physiotherapy work?
Relevance: 26%
-
Are there any exercises involved in air physiotherapy?
Relevance: 26%
-
Your pelvic health matters: insights from NHS clinicians
Relevance: 25%
-

Does air physiotherapy involve medication?
Relevance: 25%
-

NHSGGC - Respiratory Physiotherapy Service: Self-Management
Relevance: 25%
-
Who can benefit from air physiotherapy?
Relevance: 24%
-

Can air physiotherapy prevent respiratory infections?
Relevance: 24%
-

The Leeds Specialist Rehabilitation Centre - 3 Prosthetic Physiotherapy
Relevance: 24%
-
Can air physiotherapy help with COVID-19 recovery?
Relevance: 23%
-

How often should one perform air physiotherapy?
Relevance: 23%
-

Physiotherapy Exercises following an Ankle Fracture
Relevance: 23%
-

Part One: Understanding Osteoarthritis- MSK Physiotherapy
Relevance: 22%
-

How does surgery treat prostate cancer?
Relevance: 19%
-

How is PIP assessed?
Relevance: 19%
-

What is an incentive spirometer in air physiotherapy?
Relevance: 18%
-

How do I register for Self Assessment?
Relevance: 18%
-

What are the side effects of prostate cancer surgery?
Relevance: 18%
-

Who is responsible for assessing SEND needs?
Relevance: 17%
-

What is a Self Assessment tax return?
Relevance: 17%
-

Social Services and Well-being (Wales) Act: Assessments
Relevance: 16%
-

My first Self Assessment tax return
Relevance: 16%
-
Autism Assessment - What Happens in Your Appointment
Relevance: 16%
-

How do I complete my Self Assessment tax return?
Relevance: 16%
-

What is the role of mental health assessments in indefinite sentences?
Relevance: 16%
-

Are there any complications associated with untreated BPH?
Relevance: 16%
-

Can I get help from HMRC with my Self Assessment?
Relevance: 16%