Find Help
More Items From Ergsy search
-

Assessing the stroke patient
Relevance: 100%
-

Gaining consent from stroke patients
Relevance: 92%
-
Do all patients need medication to prevent heart attacks and strokes?
Relevance: 77%
-

Vale Stroke Unit
Relevance: 76%
-

Are anticoagulants effective in reducing stroke risk?
Relevance: 71%
-
Are there any recent advancements in medications for stroke prevention?
Relevance: 66%
-

Stroke - Speech and Language Therapist's Experience
Relevance: 66%
-

NHS Here for You – Stroke
Relevance: 65%
-

NHS Forth Valley’s Stroke Team
Relevance: 64%
-

Can antihypertensive medications reduce stroke risk?
Relevance: 64%
-

What role do ACE inhibitors play in stroke prevention?
Relevance: 63%
-

What drugs can reduce the risk of heart-attack and strokes?
Relevance: 58%
-

When Stroke Strikes Act F.A.S.T. | NHS
Relevance: 57%
-

Can aspirin help in reducing the risk of strokes?
Relevance: 56%
-

What is the role of lifestyle modification in heart attack and stroke prevention?
Relevance: 51%
-
Do over-the-counter medications help in preventing heart attacks and strokes?
Relevance: 49%
-

Positioning for Breathless Patient
Relevance: 40%
-

Neuroendocrine tumour patient video
Relevance: 36%
-

Sickle cell patients share their experiences.
Relevance: 36%
-

Are virtual wards suitable for elderly patients?
Relevance: 36%
-

Exercise in patients with a neuropathy
Relevance: 35%
-
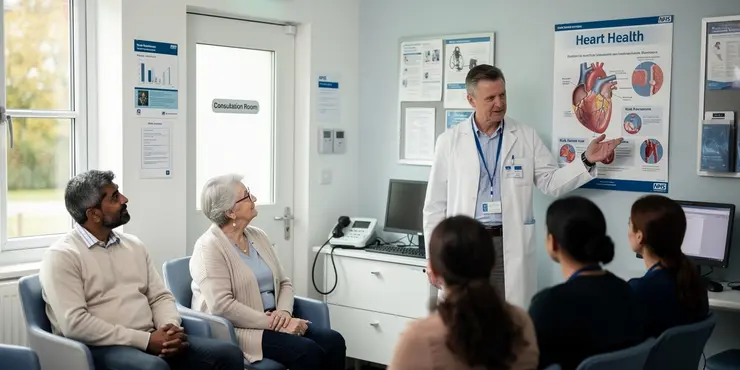
What is self-testing for eye patients?
Relevance: 35%
-

Chemotherapy - the patient journey
Relevance: 34%
-

Can technology aid in the care of Alzheimer's patients?
Relevance: 34%
-

Can Baxdrostat be used in patients with renal impairment?
Relevance: 34%
-

What types of exercise are beneficial for bowel cancer patients?
Relevance: 33%
-

What transportation services are available for Alzheimer's patients and their carers?
Relevance: 33%
-

What support is available for carers of Alzheimer's patients?
Relevance: 33%
-

Fallsafe - Put the patient first. Preventing falls in Hospital.
Relevance: 32%
-

How do virtual wards improve patient outcomes?
Relevance: 32%
-

Making a spinal brace for a scoliotic patient at the RNOH
Relevance: 32%
-
What legal resources are available for carers of Alzheimer's patients?
Relevance: 32%
-

Cornea transplant patient Information
Relevance: 32%
-

Are there online support services for prostate cancer patients on the NHS?
Relevance: 32%
-

Are there financial support programs for carers of Alzheimer's patients?
Relevance: 32%
-

Breakthrough Cancer Treatment Shows Promise for NHS Patients
Relevance: 32%
-
What if there are no NHS dentists accepting new patients?
Relevance: 32%
-

How important is self-care for carers of Alzheimer's patients?
Relevance: 32%
-

NHS Utilizes AI to Prioritize High-Risk Patients on Waiting Lists
Relevance: 32%
-

Liver transplant - Patient experience - Part 1 (Colin)
Relevance: 32%
Assessing the Stroke Patient
Initial Assessment
When assessing a stroke patient, it is crucial to act quickly and efficiently as strokes are a medical emergency. The initial assessment often begins with identifying symptoms using the FAST method: Face drooping, Arm weakness, Speech difficulties, and Time to call emergency services (999 in the UK). This quick check can be instrumental in determining whether the patient is having a stroke.Neurological Examination
A comprehensive neurological examination is essential. This involves assessing the patient’s level of consciousness, orientation, and mental status. The Glasgow Coma Scale (GCS) can be useful for this purpose. Motor skills, sensory perception, cranial nerve function, and coordination are also tested. This examination helps to establish the extent of the stroke and identify affected brain areas.Imaging Studies
Imaging studies are pivotal in stroke assessment. A CT scan is often the first imaging test conducted to distinguish between ischemic and hemorrhagic strokes. MRIs can provide more detailed images, particularly of brain tissue, and can detect early ischemic changes. These imaging results guide treatment decisions, such as thrombolytic therapy for ischemic strokes or surgical intervention for hemorrhagic strokes.Risk Factor Assessment
Understanding the patient’s risk factors is also vital. Common risk factors include hypertension, diabetes mellitus, high cholesterol, atrial fibrillation, and smoking. Assessing these factors involves reviewing the patient's medical history, conducting a physical examination, and possibly running blood tests to check lipid profiles and glucose levels. Identifying and managing these risk factors can help in both the immediate treatment and long-term management of stroke patients.Collaborative Management
Assessing a stroke patient often requires a multi-disciplinary approach. This includes consultations with neurologists, radiologists, and possibly neurosurgeons for acute care. Physiotherapists, occupational therapists, and speech and language therapists play a role in rehabilitation. Social workers and psychologists may also be involved to support the emotional and social aspects of stroke recovery. This collaborative effort ensures that all aspects of a patient’s health are addressed, improving outcomes and aiding in recovery.Monitoring and Follow-up
Continuous monitoring of the stroke patient’s vital signs, neurological status, and overall well-being is critical. Follow-up appointments should be scheduled to assess recovery progress and manage any complications. Blood pressure monitoring, lifestyle modifications, and medication adherence are often discussed during follow-up visits. Long-term rehabilitation plans may need to be adjusted based on the patient’s progress. In the UK, the National Health Service (NHS) provides a structured framework for stroke care, ensuring that patients receive timely and effective treatment across all stages of their recovery.Assessing a Stroke Patient
First Check
When checking a stroke patient, it's important to act fast. Strokes are very serious. Use the FAST method to see if someone is having a stroke: - **Face Drooping:** Is one side of the face drooping? - **Arm Weakness:** Can they lift both arms? - **Speech Problems:** Is their speech strange or hard to understand? - **Time to Act:** Call emergency services (999 in the UK) right away.Brain and Body Check
A full check of the brain and body is very important. Doctors will: - See if the person is awake and know where they are. - Check their mind using a test called the Glasgow Coma Scale (GCS). - Test their movement, senses, and how nerves in the head work. This helps to know how the stroke has affected the brain.Picture Tests
Doctors will use picture tests to look at the brain: - **CT Scan:** This is often the first test. It shows if the stroke is caused by a blocked or burst blood vessel. - **MRI:** This gives a very clear picture of the brain. It helps doctors decide on the best treatment.Risk Check
Doctors need to know what makes strokes more likely. Things like: - High blood pressure - Diabetes - High cholesterol - Smoking The doctor will look at the person’s medical history and might do blood tests. Knowing these risks helps in treating and stopping more strokes.Teamwork in Treatment
Many people work together to help stroke patients, like: - Neurologists and radiologists (brain specialists) - Surgeons - Therapists (for movement, daily tasks, and talking) - Social workers and psychologists (for emotional support) This teamwork helps patients get better.Watching and Follow-up
It's important to keep checking on the patient's health: - Regular check-ups to see how they are getting better. - Discuss changes in lifestyle and medicines. The NHS in the UK offers plans to make sure every stroke patient gets care throughout their recovery.Frequently Asked Questions
What are the common signs and symptoms of a stroke?
Common signs include sudden weakness or numbness in the face, arm, or leg, especially on one side of the body; sudden confusion or difficulty speaking; sudden trouble seeing in one or both eyes; sudden trouble walking, dizziness, loss of balance, or coordination; and sudden severe headache with no known cause.
What should I do if I suspect someone is having a stroke?
If you suspect someone is having a stroke, call 999 immediately and describe the symptoms. Act FAST: Check the Face, Arms, Speech, and Time to act fast.
What does 'Act FAST' stand for in the context of stroke?
'FAST' stands for Face (drooping), Arms (weakness), Speech (difficulty), and Time (to call emergency services).
How is a stroke diagnosed?
Stroke is diagnosed through a combination of medical history, physical exams, and imaging tests such as CT scans, MRI scans, and sometimes ultrasound of the carotid arteries.
What are the different types of stroke?
The main types are ischemic stroke, caused by a blockage or clot in a blood vessel, and haemorrhagic stroke, caused by bleeding in or around the brain.
What are transient ischemic attacks (TIAs)?
TIAs, or mini-strokes, are temporary periods of symptoms similar to those of a stroke. They are caused by a short-term disruption in blood supply to the brain and are a warning sign of a possible future stroke.
Is it important to recognise and treat strokes quickly?
Yes, immediate medical treatment can significantly reduce the risk of long-term disability and increase the chances of recovery.
What treatments are available for stroke patients?
Treatments include clot-busting drugs for ischemic stroke, surgery to remove blood clots, or repair broken blood vessels, and supportive therapies such as rehabilitation.
Can lifestyle changes help prevent strokes?
Yes, maintaining a healthy lifestyle with regular exercise, a balanced diet, not smoking, and controlling blood pressure, cholesterol, and diabetes can help reduce the risk of strokes.
Are there specific medications to manage stroke risk?
Medications such as antiplatelets (aspirin), anticoagulants (warfarin), blood pressure medications, and cholesterol-lowering drugs may be prescribed to manage stroke risk.
How does rehabilitation help in stroke recovery?
Rehabilitation helps patients regain lost skills, relearn basic tasks, and improve physical, emotional, and cognitive well-being through physical therapy, occupational therapy, and speech therapy.
Can strokes cause permanent disability?
Yes, strokes can lead to long-term disabilities, depending on the severity and location of the brain affected. Early treatment and rehabilitation can improve outcomes.
Is stroke more common in older adults?
Yes, stroke risk increases with age, especially after age 55, but it can occur at any age.
Are there genetic factors associated with stroke risk?
Yes, a family history of stroke can increase an individual’s risk, but lifestyle and health factors play a larger role.
What role does high blood pressure play in stroke risk?
High blood pressure is the most significant risk factor for stroke, as it can damage blood vessels, leading to either blockage or rupture.
What are the common signs of a stroke?
Look for these signs of a stroke:
- Face: One side of the face may droop or feel numb. Ask the person to smile.
- Arms: One arm may be weak or numb. Ask the person to raise both arms. Does one drift down?
- Speech: Speech may be slurred or strange. Ask the person to repeat a simple sentence, like "The sky is blue."
- Time: If you see any of these signs, call for help fast. Use a phone to call your emergency number.
Helpful tip: You can use a pen and paper to write down the signs you see.
Here are some things to watch out for: if someone suddenly feels weak or numb in their face, arm, or leg, especially on one side of their body. They might get confused or have a hard time talking. They might have trouble seeing with one or both eyes. Walking might be hard because they feel dizzy or lose their balance. They might also get a really bad headache for no reason.
If you see these signs, you can help by calling for help right away. Also, talk to a grown-up you trust. There are tools like picture cards or apps that might help explain these signs. Practicing with someone else can make it easier to remember.
What to Do If You Think Someone Has a Stroke
A stroke is when the brain is not getting enough blood. This can be very serious.
If you think someone is having a stroke, follow these steps:
- Call Help: Phone an ambulance right away. Dial emergency services.
- Use F.A.S.T: This is a way to remember the signs:
- Face: Ask the person to smile. Does one side of their face droop?
- Arms: Ask the person to raise both arms. Does one arm drift down?
- Speech: Ask the person to say a simple sentence. Are the words slurred or hard to understand?
- Time: If you see any of these signs, call for help fast!
Stay with the person until help arrives.
Use tools like a watch with a timer or an app on your phone to note the time when signs started.
If you think someone is having a stroke, call 999 right away. Tell them what you see. Remember FAST: Look at their Face, Arms, Speech, and it's Time to get help fast.
What does 'Act FAST' mean when talking about a stroke?
'Act FAST' is a way to remember the signs of a stroke and what to do.
- F is for Face: Can the person smile? Does one side of the face droop?
- A is for Arms: Can the person lift both arms? Is one arm weak?
- S is for Speech: Can the person talk clearly? Is their speech slurred?
- T is for Time: If you see any of these signs, call for help fast!
If you find these signs, use a phone to call for help.
'FAST' helps you remember signs of a stroke. It stands for:
Face: Check if their face is drooping on one side.
Arms: See if one arm feels weak or can't be lifted.
Speech: Listen for slurred or strange speech.
Time: Call emergency services right away if you see these signs.
You can use tools like picture cards to help remember. Practice with someone to learn it well.
How do doctors know if someone had a stroke?
Doctors check if someone had a stroke by doing special tests.
First, they talk to the person and ask questions.
Then, they might do a scan of the brain. This is called a "CT scan" or "MRI." It takes a picture of the inside of the head.
To help understand, doctors use simple words and pictures. Family or friends can help explain too.
You can also use apps or videos that help explain stroke with easy words or games.
Doctors find out if someone had a stroke by asking questions, checking the body, and using special pictures like CT scans, MRI scans, and sometimes an ultrasound of the neck.
Here are some tools or ideas to help understand this:
- Pictures: Use simple pictures of a doctor's visit. This can help show what doctors do to find out if someone had a stroke.
- Videos: Watch a short video that explains strokes in easy words.
- Talking with Someone: Talk with a family member or friend who can explain it in your own words.
What are the different types of stroke?
A stroke is a problem in the brain. It happens when blood can't get to the brain.
There are two main types of stroke:
- Ischemic Stroke: This happens when something blocks the blood flow to the brain.
- Hemorrhagic Stroke: This happens when a blood vessel in the brain breaks and bleeds.
If you want more help, you can use tools that read text out loud. You can also talk to someone who knows about strokes to learn more.
The two main types of strokes are:
- Ischemic stroke: This happens when something blocks the blood flow in a blood vessel.
- Haemorrhagic stroke: This happens when there is bleeding in or around the brain.
To help understand strokes better, you might find tools like picture charts or videos useful.
What are transient ischemic attacks (TIAs)?
TIAs are sometimes called "mini-strokes." They happen when blood flow to the brain is blocked for a short time. This can cause brief stroke-like symptoms, but they don't last long. It's important to tell a doctor if you think you had a TIA.
To understand better, you can use pictures or watch videos about TIAs. These tools can help you learn more easily.
TIAs, or mini-strokes, happen when the brain does not get enough blood for a short time. This can make a person feel like they are having a stroke, but the feeling goes away. TIAs are a warning sign that a real stroke might happen later.
Why is it important to help someone with a stroke right away?
A stroke happens when part of the brain doesn’t get enough blood. This can be very serious.
It is very important to help quickly if someone has a stroke. This can stop more harm and help them get better.
Here are some things to do if you think someone is having a stroke:
- Face: Ask the person to smile. Is one side of the face droopy?
- Arms: Ask the person to raise both arms. Is one arm weak or numb?
- Speech: Ask the person to say a simple sentence. Are the words slurred or hard to understand?
- Time: If you see any of these signs, call for help right away.
You can also use pictures or ask someone to help explain this. Remember, acting fast can help a lot!
Yes, getting medical help right away can help you get better and stop serious problems later. It can make it easier for you to recover.
What treatments can help people who have had a stroke?
If someone has a stroke, doctors can help them get better in different ways.
Here are some treatments:
- Medicines: These can help to make people feel better.
- Therapy: Talking and exercises can help people move and speak better.
- Hospital Care: Nurses and doctors take care of patients to help them recover.
Tools to help:
- Ask a friend or family member to help explain things.
- Use pictures or videos to understand more about strokes.
Treatments help make you feel better after a stroke. There are different ways to help:
- Special medicine that helps clear blood clots. It’s like medicine superheroes for your blood!
- Doctors can do surgery to take out blood clots. They can also fix broken blood tubes.
- There are other ways to help, like special exercises to help you get strong again. This is called rehabilitation.
Can changing your habits stop a stroke?
Yes, staying healthy can help you avoid strokes. Here are some things you can do:
- Exercise regularly. Try to move your body every day.
- Eat a balanced diet. This means eating fruits, vegetables, and other healthy foods.
- Don't smoke. Smoking is bad for your health.
- Check your blood pressure. High blood pressure can be dangerous.
- Know your cholesterol levels. Keep them in a healthy range.
- If you have diabetes, make sure to control it with your doctor's help.
If reading is hard, you can use tools like audiobooks or ask someone to read with you. It's okay to ask for help!
Are there medicines to help prevent a stroke?
Yes, there are medicines that can help stop strokes. Doctors give these medicines to keep your blood flowing well. Here are some types of medicines:
- Blood thinners: These make your blood less sticky. They help stop clots that can cause a stroke.
- Blood pressure medicine: High blood pressure can cause strokes. This medicine helps keep your blood pressure normal.
- Cholesterol medicine: Cholesterol is a type of fat in your blood. Too much can cause a stroke. This medicine lowers cholesterol.
Doctors will talk with you to find the right medicine. It's important to take medicine just like the doctor says.
If you find it hard to understand, ask someone to help you read or talk to your doctor. You can also use voice-to-text apps to hear the information.
Doctors might give you medicine to help lower your risk of a stroke. Some of these medicines are:
- Aspirin: It helps stop blood clots.
- Warfarin: It also helps prevent blood clots.
- Blood pressure medicine: It keeps your blood pressure in control.
- Cholesterol medicine: It helps lower cholesterol levels.
If you want more help to remember things, you can use a calendar or set alarms on your phone.
How does rehabilitation help someone get better after a stroke?
Rehabilitation is a way to help people get back skills they lost. It helps them learn how to do simple things again. It also helps them feel better in their body, mind, and emotions. This is done through physical exercises, daily activity practice, and talking exercises.
If you find it hard to read, you can try using tools that read the words out loud or show the text in bigger letters. You can also ask someone you trust to read it with you and help explain the words.
Can a stroke cause lasting problems?
A stroke can hurt your brain.
This might make it hard to move, talk, or remember things.
Some problems can last for a long time.
Tools like pictures and simple words can help people understand better.
Yes, having a stroke can cause problems that do not go away. It depends on how serious the stroke is and what part of the brain it happens in. Getting help quickly and doing special exercises can make you feel better.
Do more older people have strokes?
Yes, the chance of having a stroke goes up as you get older, especially after you turn 55. But a stroke can happen at any age.
Can genes make you more likely to have a stroke?
If people in your family have had a stroke, you might have a higher chance of having one too. But how you live and take care of your health is even more important.
How does high blood pressure cause a stroke?
High blood pressure is when there is too much force in your blood pushing against your blood vessels.
This can hurt your blood vessels and can lead to a stroke.
A stroke happens when blood can’t reach parts of your brain.
Using a blood pressure monitor can help you track your blood pressure and keep it healthy.
Having high blood pressure is very risky for getting a stroke. It can hurt the blood tubes in your body, causing them to get blocked or burst.
Here are some tips to help understand this better:
- Think of blood tubes like water pipes. If they get blocked or break, it can cause problems.
- Tools like picture cards or videos can help explain how blood pressure works.
- Ask a friend or adult to explain any tricky words.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Assessing the stroke patient
Relevance: 100%
-

Gaining consent from stroke patients
Relevance: 92%
-
Do all patients need medication to prevent heart attacks and strokes?
Relevance: 77%
-

Vale Stroke Unit
Relevance: 76%
-

Are anticoagulants effective in reducing stroke risk?
Relevance: 71%
-
Are there any recent advancements in medications for stroke prevention?
Relevance: 66%
-

Stroke - Speech and Language Therapist's Experience
Relevance: 66%
-

NHS Here for You – Stroke
Relevance: 65%
-

NHS Forth Valley’s Stroke Team
Relevance: 64%
-

Can antihypertensive medications reduce stroke risk?
Relevance: 64%
-

What role do ACE inhibitors play in stroke prevention?
Relevance: 63%
-

What drugs can reduce the risk of heart-attack and strokes?
Relevance: 58%
-

When Stroke Strikes Act F.A.S.T. | NHS
Relevance: 57%
-

Can aspirin help in reducing the risk of strokes?
Relevance: 56%
-

What is the role of lifestyle modification in heart attack and stroke prevention?
Relevance: 51%
-
Do over-the-counter medications help in preventing heart attacks and strokes?
Relevance: 49%
-

Positioning for Breathless Patient
Relevance: 40%
-

Neuroendocrine tumour patient video
Relevance: 36%
-

Sickle cell patients share their experiences.
Relevance: 36%
-

Are virtual wards suitable for elderly patients?
Relevance: 36%
-

Exercise in patients with a neuropathy
Relevance: 35%
-
What is self-testing for eye patients?
Relevance: 35%
-

Chemotherapy - the patient journey
Relevance: 34%
-

Can technology aid in the care of Alzheimer's patients?
Relevance: 34%
-

Can Baxdrostat be used in patients with renal impairment?
Relevance: 34%
-

What types of exercise are beneficial for bowel cancer patients?
Relevance: 33%
-

What transportation services are available for Alzheimer's patients and their carers?
Relevance: 33%
-

What support is available for carers of Alzheimer's patients?
Relevance: 33%
-

Fallsafe - Put the patient first. Preventing falls in Hospital.
Relevance: 32%
-

How do virtual wards improve patient outcomes?
Relevance: 32%
-

Making a spinal brace for a scoliotic patient at the RNOH
Relevance: 32%
-
What legal resources are available for carers of Alzheimer's patients?
Relevance: 32%
-

Cornea transplant patient Information
Relevance: 32%
-

Are there online support services for prostate cancer patients on the NHS?
Relevance: 32%
-

Are there financial support programs for carers of Alzheimer's patients?
Relevance: 32%
-

Breakthrough Cancer Treatment Shows Promise for NHS Patients
Relevance: 32%
-
What if there are no NHS dentists accepting new patients?
Relevance: 32%
-

How important is self-care for carers of Alzheimer's patients?
Relevance: 32%
-

NHS Utilizes AI to Prioritize High-Risk Patients on Waiting Lists
Relevance: 32%
-

Liver transplant - Patient experience - Part 1 (Colin)
Relevance: 32%