Find Help
More Items From Ergsy search
-

Clinical Handover - Care 24/7
Relevance: 100%
-

Fracture Clinic: Plaster Casts
Relevance: 27%
-

Clinical depression: Lawrence's story | NHS
Relevance: 26%
-

Dementia Care at Colten Care
Relevance: 25%
-
How do clinics determine if IVF is the right option?
Relevance: 24%
-

Are there any clinical trials supporting Ozempic for weight loss?
Relevance: 24%
-

Post Menopausal Bleeding Clinic | A Guide to What Happens at An Appointment
Relevance: 23%
-
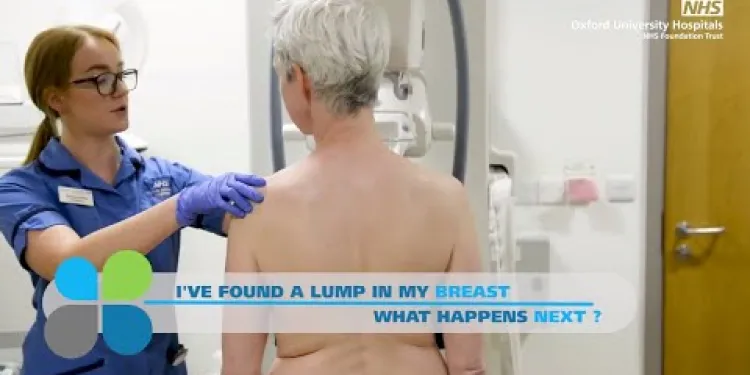
I've found a lump in my breast - What happens next? The breast diagnostic clinic
Relevance: 23%
-
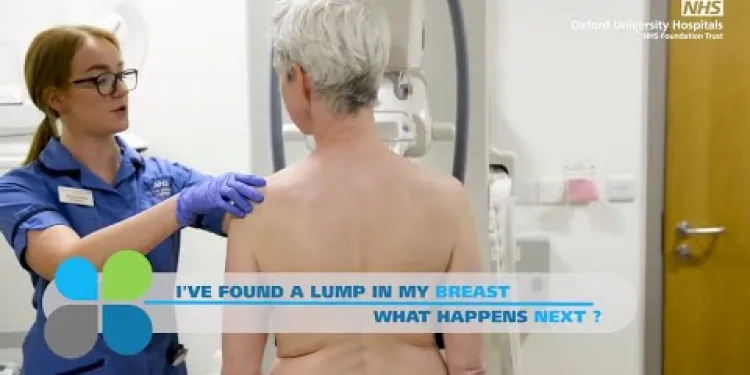
I've found a lump in my breast - What happens next? The breast diagnostic clinic
Relevance: 23%
-

Chiropractic Care on the NHS
Relevance: 23%
-
Stoma Care
Relevance: 21%
-

Personal Health: Navigating the NHS for Efficient Care
Relevance: 21%
-

Derbyshire Diabetic Eye Screening - Assessment Clinic Appointment
Relevance: 21%
-

Neck Care Exercises
Relevance: 20%
-

What is end of life care?
Relevance: 20%
-

The role of care homes dedicated to caring for people living with dementia and memory loss
Relevance: 20%
-
Self care for your feet - Podiatrist
Relevance: 20%
-

NHS Acute Care Anaphylaxis
Relevance: 19%
-

Amberwood House (Colten Care)
Relevance: 19%
-

Birchgrove - Assisted-living accommodation and care
Relevance: 19%
-

Dr Hilary Jones on Residential Care PART 2.
Relevance: 19%
-

Dr Hilary Jones on Residential Care PART 1.
Relevance: 19%
-

Child Care Proceedings | Family Law
Relevance: 19%
-

Can chiropractic care help with arthritis?
Relevance: 19%
-

How can I plan for future care needs?
Relevance: 18%
-

Can children benefit from chiropractic care?
Relevance: 18%
-

Is chiropractic care covered by insurance?
Relevance: 18%
-

Preventative Care: What Your Family Needs
Relevance: 18%
-

Diabetes Care - Preventing Amputations
Relevance: 17%
-

Colten Care values - montage of all 5 short films
Relevance: 17%
-

How do I know if I'm eligible for free NHS dental care?
Relevance: 17%
-

Animation - Primary care and NHS 111
Relevance: 17%
-

Fernhill Dedicated Dementia Care Home - a relatives perspective
Relevance: 17%
-

Transforming Care for people with Learning Disabilities and/ or Autism: Peter's Story
Relevance: 17%
-

Self care - sunburn
Relevance: 17%
-

Knee Care Exercises
Relevance: 17%
-

What is an Education, Health and Care Plan (EHCP)?
Relevance: 16%
-

Dr Hilary Jones shares his professional and personal thoughts on Colten Care
Relevance: 16%
-

How the Shortage of GPs is Affecting Patient Care Across the UK
Relevance: 16%
-

Self care - sunburn
Relevance: 16%
Clinical Handover - Care 24/7
Importance of Clinical Handover
Clinical handover, also known as shift handover, is a critical process in healthcare settings, ensuring continuity of care 24/7. It involves the transfer of patient information, responsibility, and accountability from one healthcare professional to another. Effective handover is vital to maintaining patient safety and quality of care, reducing the risk of errors, and ensuring all relevant data is conveyed accurately.
Best Practices for Effective Handover
For clinical handover to be effective, structured communication is key. In the UK, the SBAR (Situation-Background-Assessment-Recommendation) tool is widely used to standardize this process. Clear, concise, and comprehensive documentation, face-to-face handover sessions, and the use of checklists are recommended best practices. Ensuring that all team members, including nurses, doctors, and allied health professionals, are trained in these methods is crucial for maintaining high standards of care.
Challenges in 24/7 Care
Providing continuous care around the clock presents challenges, including managing staff fatigue, maintaining high standards of communication during shift changes, and ensuring that all healthcare professionals are up-to-date with the latest patient information. In the UK, the National Health Service (NHS) places significant emphasis on addressing these challenges through robust training programmes and stringent policies to facilitate smooth handover processes.
Technological Support for Clinical Handover
Advancements in technology have significantly improved clinical handover processes. Electronic Health Records (EHRs) allow for real-time updating and easy access to patient information, which aids in seamless transitions between shifts. Mobile apps and secure communication platforms also facilitate quick and effective communication among healthcare professionals, ensuring that vital information is conveyed promptly. In the UK, digital solutions are increasingly being adopted to enhance the efficiency and reliability of clinical handover.
Conclusion
In the UK, clinical handover is an essential component of patient care, ensuring safety and continuity of service 24/7. By adhering to structured communication tools like SBAR, implementing best practices, overcoming inherent challenges, and embracing technological advancements, healthcare providers can significantly improve the handover process and contribute to better patient outcomes.
Clinical Handover - Care 24/7
Why Clinical Handover is Important
Clinical handover happens when one healthcare worker gives patient information to another. This is important to make sure the care continues all day and night. It's crucial for keeping patients safe and making sure they get good care.
How to Do a Good Handover
To make handover work well, we need clear communication. In the UK, many people use a tool called SBAR. This helps healthcare workers share important information in a clear way. Writing things down, talking face-to-face, and using checklists can help. Training all healthcare workers, like nurses and doctors, is very important.
Challenges in 24/7 Care
Providing care all the time can be hard. Workers might get tired, and they need to make sure everyone knows the latest patient information. In the UK, the NHS has training and rules to help with these challenges.
How Technology Can Help
Technology has made handovers better. Electronic Health Records (EHRs) help keep patient information updated and easy to share. Apps and secure chat systems let healthcare workers talk quickly. In the UK, more digital tools are used to make handovers better and safer.
Summary
In the UK, clinical handover is very important. It keeps patients safe and their care going round the clock. Using tools like SBAR, learning best practices, and using new technologies helps improve this process.
Frequently Asked Questions
What is the purpose of clinical handover?
The purpose of clinical handover is to ensure the continuity of care and the safety of patients by effectively transferring crucial clinical information between healthcare providers.
Who is responsible for conducting clinical handovers?
Clinical handovers are typically conducted by healthcare professionals such as doctors, nurses, and allied health workers involved in the patient's care.
When should a clinical handover take place?
Clinical handovers should take place at any transition of care, such as shift changes, patient transfers between departments, and discharge to another facility.
What information should be included in a clinical handover?
Key information to include in a clinical handover comprises the patient's current condition, medical history, treatment plans, ongoing care needs, and any critical issues or precautions.
How long does a typical clinical handover last?
The duration of a clinical handover can vary but typically lasts between 5 to 15 minutes, depending on the complexity of the patient's condition and the amount of information that needs to be conveyed.
What is SBAR and how is it used in clinical handovers?
SBAR stands for Situation, Background, Assessment, Recommendation. It is a structured communication tool used to ensure clear and concise transfer of information during clinical handovers.
Why is clinical handover important for patient safety?
Clinical handovers are crucial for patient safety as they help prevent miscommunication, reduce the risk of errors, and ensure that all healthcare providers are aware of the patient's current status and care needs.
How can electronic health records (EHR) improve clinical handovers?
Electronic health records can improve clinical handovers by providing real-time access to patient information, reducing the risk of information loss, and facilitating better coordination among healthcare providers.
What are some common challenges in clinical handovers?
Common challenges in clinical handovers include time constraints, communication barriers, incomplete information, and lack of standardisation in the handover process.
Can family members be involved in clinical handovers?
Yes, involving family members in clinical handovers can provide a more comprehensive understanding of the patient's needs and ensure that they are aware of the care plan and any necessary follow-up actions.
What role do multidisciplinary team meetings play in clinical handovers?
Multidisciplinary team meetings facilitate coordinated care through detailed discussions among various healthcare professionals, ensuring that all aspects of the patient's condition are considered and addressed during handovers.
How is patient confidentiality maintained during clinical handovers?
Patient confidentiality is maintained by conducting handovers in private settings, ensuring that only relevant healthcare professionals are present and adhering to data protection guidelines and regulations.
What training resources are available for improving clinical handover skills?
Training resources for improving clinical handover skills include workshops, online modules, simulation exercises, and specific communication training programs.
How do clinical handovers differ in different healthcare settings?
Clinical handovers may vary between healthcare settings such as hospitals, primary care, and community care based on the specific needs and dynamics of each environment.
What are the key indicators of a successful clinical handover?
Key indicators of a successful clinical handover include clear and concise communication, accurate and complete information transfer, understanding of the care plan, and improved patient outcomes.
Why do doctors and nurses share patient information?
When doctors and nurses change shifts, they need to talk about each patient. This is called a "handover." The goal is to make sure every patient is safe and gets the right care.
Who is responsible for clinical handovers?
Who should do clinical handovers?
Clinical handovers are when doctors and nurses share information about a patient.
It is important so that everyone knows the patient's needs.
Doctors and nurses are responsible for doing handovers.
Tools to help:
- Ask questions if you do not understand.
- Use a notepad to write down important details.
- Speak slowly and clearly.
Doctors, nurses, and other health workers talk to each other about how to care for the patient. This is called a clinical handover.
When should doctors and nurses share information?
Doctors and nurses should talk to each other when they change shifts. This helps them share important information about patients. They should also do this before a patient moves to a new place or when their care changes.
Supportive tools to help understand this:
- Use pictures to show when handovers happen.
- Ask someone to explain if you're unsure.
Doctors and nurses should talk to each other whenever they change who is taking care of a patient. This should happen when shifts change, when a patient moves to a different department in the hospital, or when a patient leaves to go to another place.
What information should be included in a clinical handover?
When doctors and nurses change shifts, they do something called a "clinical handover." This is like telling a story about how a patient is doing. Do you know what needs to be in this story? Here are the important parts:
- Name and Details: The person's name, age, and any important details about them.
- Health Problem: What is making the person sick or hurt? What's their main health problem?
- Treatment Plan: What are the doctors and nurses doing to help the person get better? What medicine or care are they giving?
- Changes: Did anything new happen with the person’s health? Did they get better or worse?
- Next Steps: What do the doctors and nurses need to do next to help the person? What should the next doctor or nurse know?
To help remember all these parts, you can use a checklist. A checklist is a tool that helps you make sure you don’t forget anything important. Also, speaking clearly and writing things down can help make sure everyone knows what to do.
When doctors and nurses talk about a patient, they need to share important information. This includes:
- How the patient is feeling right now.
- What health problems the patient has had before.
- The medicine or treatment the patient is getting.
- What the patient needs to feel better.
- Anything extra important or things to be careful about.
Using pictures or simple charts can help. Asking questions if you’re unsure can also be useful.
How long is a usual clinical handover?
A clinical handover is a time when doctors and nurses share important information about a patient.
This usually takes about 5 to 10 minutes.
You can use tools like timers to help keep track of time.
A clinical handover usually takes about 5 to 15 minutes. How long it takes depends on how complex the patient's condition is and how much information needs to be shared.
What is SBAR and how do people use it in clinical handovers?
SBAR is a way for doctors and nurses to talk to each other.
It helps them share important information fast.
SBAR stands for:
- S - Situation: What is happening right now?
- B - Background: What happened before?
- A - Assessment: What do you think is wrong?
- R - Recommendation: What do you want to happen next?
Doctors and nurses use SBAR to make sure everyone knows what is going on with a patient.
SBAR helps keep patients safe by making sure everyone has the same information.
A tool that can help with using SBAR is writing things down clearly.
This helps people remember what to say during a handover.
SBAR helps people share important information the right way. It stands for:
- **Situation**: What is happening right now?
- **Background**: What happened before?
- **Assessment**: What do we think is wrong?
- **Recommendation**: What should we do next?
Using SBAR makes sure everyone understands what's going on, especially when doctors and nurses change shifts.
Try drawing pictures or using voice recordings to help understand and remember SBAR better.
Why is it important for doctors and nurses to share information about patients?
Sharing information is important to keep patients safe. When doctors and nurses talk to each other about a patient, they all know what care the patient needs. This makes sure nothing is forgotten or left out.
Here are some tips to help understand why this is important:
- Ask questions if you don't understand.
- Use pictures or drawings to help explain.
- Talk to someone you trust about what you learned.
Passing important information from one doctor or nurse to another is very important. This helps keep patients safe. It makes sure that everyone knows what is happening with the patient's care. It stops mistakes from happening.
How can electronic health records (EHR) make patient handovers better?
Doctors and nurses sometimes need to pass on important patient information. This is called a handover. Electronic health records, or EHR, can help with this.
EHR can store all the patient's information in one place. This means doctors and nurses can quickly find and share what they need to know.
Having EHR can stop mistakes. It makes sure that every person caring for the patient has the right information.
EHR can also save time. Doctors and nurses don't have to write everything down by hand. They can use the computer instead.
Using pictures or symbols can help people understand the information better. Reading tools can also be helpful for everyone to stay informed.
Electronic health records help doctors and nurses share patient information. This helps people work together better and makes sure important information is not lost. This is a good way to keep patients safe and healthy.
What problems happen when doctors and nurses share patient information?
When doctors and nurses change shifts, they need to tell each other important information. This is called a handover. Some things can make handovers hard. These include not having enough time, having trouble talking clearly, missing information, and not having a set way to do the handover.
To make handovers better, you can try using checklists and speaking slowly. You can also use a voice recorder to make sure you remember what is said. These tools can help everyone understand and share important details.
Can family members help when doctors and nurses share patient information?
When doctors and nurses talk about a patient's care, it is called a "clinical handover." Family members can sometimes be there to listen and help. This can make sure everyone's on the same page.
It helps if family members ask questions if they don't understand. They can also write things down to remember important details.
Using picture charts or simple notes can make it easier for everyone to understand what's happening. This way, family knows how they can support the patient best.
Yes, it is good to include family members when doctors and nurses talk about how to take care of a patient. This helps everyone understand what the patient needs and what to do next.
How do team meetings help doctors and nurses share information?
Doctors, nurses, and other health workers have meetings to talk about patients. These meetings are called team meetings. Team meetings help everyone share important information about patients.
At these meetings, health workers talk about what care the patient needs. They make sure everyone knows what to do to help the patient get better.
Using pictures or drawing can make the information easier to understand. You can also ask someone to explain things if you find it difficult.
Team meetings help doctors and nurses share important information. These meetings make sure everyone knows what the patient needs. This way, patients get the best care.
How do doctors keep patient information private when talking to each other?
Doctors and nurses sometimes need to share your health information to help you. It is important they do this safely:
- They talk where others can't hear.
- They only tell people who need to know.
- They use secure computers.
If you have questions or feel worried, you can:
- Ask your doctor to explain.
- Tell them if you are concerned about privacy.
We keep patient information private by talking about it in quiet places. Only the right doctors and nurses are there. We also follow rules to protect personal details.
What Can Help Me Get Better at Passing Patient Information?
Here are some ways you can practice:
- Watch videos that show how to pass patient information.
- Play games that help you remember what to say.
- Use a checklist to make sure you say everything important.
- Practice with a friend or helper to get better.
Here are ways to get better at handing over patient information:
- Attend workshops. These are like classes where you can learn new things.
- Try online modules. These are lessons you can find on the computer.
- Do practice exercises with others. You pretend to hand over information to learn how to do it well.
- Join communication training programs. These programs help you talk and share information better.
Using these tools can help you improve your skills.
What are clinical handovers like in different places?
When doctors and nurses change shifts, they tell each other important information. This is called a "handover."
In hospitals, handovers might happen at a patient's bedside. In a clinic, they might talk in an office.
In different places, handovers can be done in different ways.
To understand better, you can use pictures or ask someone to explain it to you.
Doctors and nurses share important information when they change shifts or patients move to different places like hospitals or clinics. Each place has its own needs and ways of doing things.
How can we tell if a clinical handover is good?
Things to look for in a good handover in hospitals:
- Everyone talks clearly and simply.
- All important information is shared.
- Everyone understands the care plan.
- Patients get better care.
To help with understanding:
- Use short sentences when talking.
- Repeat important points.
- Ask questions if you don’t understand.
Useful Links
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Clinical Handover - Care 24/7
Relevance: 100%
-

Fracture Clinic: Plaster Casts
Relevance: 27%
-

Clinical depression: Lawrence's story | NHS
Relevance: 26%
-

Dementia Care at Colten Care
Relevance: 25%
-
How do clinics determine if IVF is the right option?
Relevance: 24%
-

Are there any clinical trials supporting Ozempic for weight loss?
Relevance: 24%
-

Post Menopausal Bleeding Clinic | A Guide to What Happens at An Appointment
Relevance: 23%
-
I've found a lump in my breast - What happens next? The breast diagnostic clinic
Relevance: 23%
-
I've found a lump in my breast - What happens next? The breast diagnostic clinic
Relevance: 23%
-

Chiropractic Care on the NHS
Relevance: 23%
-
Stoma Care
Relevance: 21%
-

Personal Health: Navigating the NHS for Efficient Care
Relevance: 21%
-

Derbyshire Diabetic Eye Screening - Assessment Clinic Appointment
Relevance: 21%
-

Neck Care Exercises
Relevance: 20%
-

What is end of life care?
Relevance: 20%
-

The role of care homes dedicated to caring for people living with dementia and memory loss
Relevance: 20%
-
Self care for your feet - Podiatrist
Relevance: 20%
-

NHS Acute Care Anaphylaxis
Relevance: 19%
-

Amberwood House (Colten Care)
Relevance: 19%
-

Birchgrove - Assisted-living accommodation and care
Relevance: 19%
-

Dr Hilary Jones on Residential Care PART 2.
Relevance: 19%
-

Dr Hilary Jones on Residential Care PART 1.
Relevance: 19%
-

Child Care Proceedings | Family Law
Relevance: 19%
-

Can chiropractic care help with arthritis?
Relevance: 19%
-

How can I plan for future care needs?
Relevance: 18%
-

Can children benefit from chiropractic care?
Relevance: 18%
-

Is chiropractic care covered by insurance?
Relevance: 18%
-

Preventative Care: What Your Family Needs
Relevance: 18%
-

Diabetes Care - Preventing Amputations
Relevance: 17%
-

Colten Care values - montage of all 5 short films
Relevance: 17%
-

How do I know if I'm eligible for free NHS dental care?
Relevance: 17%
-

Animation - Primary care and NHS 111
Relevance: 17%
-

Fernhill Dedicated Dementia Care Home - a relatives perspective
Relevance: 17%
-

Transforming Care for people with Learning Disabilities and/ or Autism: Peter's Story
Relevance: 17%
-

Self care - sunburn
Relevance: 17%
-

Knee Care Exercises
Relevance: 17%
-

What is an Education, Health and Care Plan (EHCP)?
Relevance: 16%
-

Dr Hilary Jones shares his professional and personal thoughts on Colten Care
Relevance: 16%
-

How the Shortage of GPs is Affecting Patient Care Across the UK
Relevance: 16%
-

Self care - sunburn
Relevance: 16%