Find Help
More Items From Ergsy search
-

Evidence-Based Interventions: snoring surgery in the absence of Obstructive Sleep Apnoea (OSA)
Relevance: 100%
-

Is snoring always a sign of sleep apnea?
Relevance: 89%
-

What is sleep apnea?
Relevance: 77%
-

What is sleep apnoea?
Relevance: 76%
-
What causes obstructive sleep apnea?
Relevance: 75%
-

How common is sleep apnea?
Relevance: 71%
-

What are the main types of sleep apnea?
Relevance: 71%
-

Does sleep apnea occur only in adults?
Relevance: 69%
-
What is complex sleep apnea syndrome?
Relevance: 67%
-
Introduction to obstructive sleep apnoea
Relevance: 66%
-

Is CPAP the only treatment for sleep apnea?
Relevance: 64%
-

Why is sleep apnea dangerous?
Relevance: 62%
-

What are common symptoms of sleep apnea?
Relevance: 62%
-
Can weight loss improve sleep apnea?
Relevance: 61%
-
What treatments are available for sleep apnea?
Relevance: 61%
-
How is sleep apnea diagnosed?
Relevance: 60%
-

What is complex sleep apnea syndrome?
Relevance: 60%
-

Can alcohol worsen sleep apnea?
Relevance: 59%
-

Can children have sleep apnea?
Relevance: 57%
-

Can sleep apnea be cured?
Relevance: 57%
-

What should I do if I suspect I have sleep apnea?
Relevance: 57%
-

What lifestyle changes can help manage sleep apnea?
Relevance: 52%
-

Am I eligible to try the new sleep apnea chip?
Relevance: 51%
-

What are risk factors for developing sleep apnea?
Relevance: 51%
-
How does the new Sleep Apnea Chip work?
Relevance: 46%
-

How does central sleep apnea differ from obstructive sleep apnea?
Relevance: 34%
-
Evidence-Based Interventions: tonsillectomy for recurrent tonsillitis surgery
Relevance: 32%
-

Weight Loss Surgery
Relevance: 29%
-
What is sleep apnoea?
Relevance: 26%
-

Is surgery necessary for Crohn's disease?
Relevance: 24%
-

What are the risks associated with baby sleep pillows?
Relevance: 23%
-

What is the safest sleep environment for an infant?
Relevance: 23%
-

Why are baby sleep pillows not safe for infants?
Relevance: 22%
-

Are baby sleep pillows safe?
Relevance: 22%
-

Prostate Surgery
Relevance: 21%
-

The Importance of Sleep for All Ages
Relevance: 21%
-

A journey to hip surgery
Relevance: 21%
-

Are there any benefits to using baby sleep pillows?
Relevance: 21%
-

How does sleep quality relate to menopause symptoms?
Relevance: 21%
-

Do crib wedges pose the same risks as baby sleep pillows?
Relevance: 20%
Evidence-Based Interventions: Snoring Surgery in the Absence of Obstructive Sleep Apnoea (OSA)
Introduction to Snoring
Snoring is a common condition characterized by noisy breathing during sleep. While often considered a mere nuisance, it can lead to disturbed sleep for both the individual affected and their partner. In the absence of Obstructive Sleep Apnoea (OSA), where snoring isn't associated with significant airway obstruction, various interventions, including surgery, may be considered to alleviate the problem.Understanding Non-OSA Snoring
Non-OSA snoring happens when there is vibration of the structures of the upper airway, such as the soft palate and uvula, without significant airway obstruction that characterizes OSA. It can be influenced by factors like nasal congestion, obesity, alcohol consumption, and sleeping position. In the UK, non-OSA snoring is recognized as both a medical and social concern due to its impact on sleep quality and relationships.When to Consider Surgery for Snoring
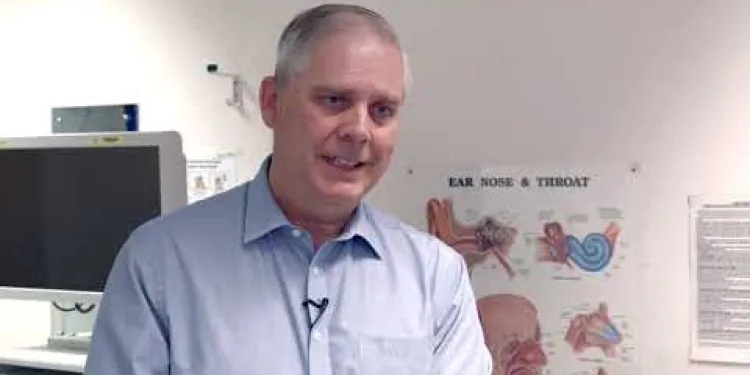
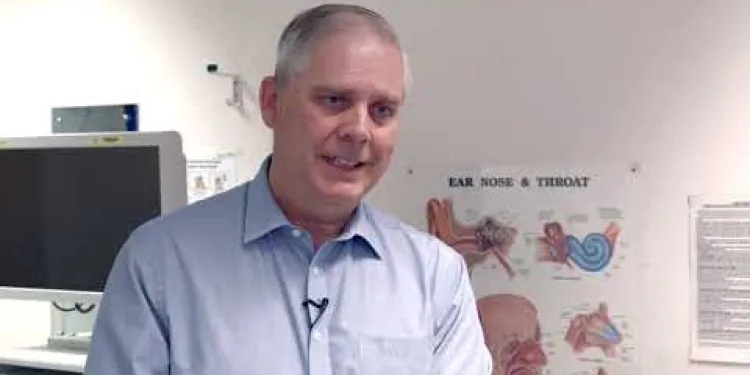
Surgery for snoring in the absence of OSA is generally considered when conservative measures, such as lifestyle changes and continuous positive airway pressure (CPAP) therapy, prove ineffective. Patients who do not respond to these interventions and experience significant impairment in their quality of life may be candidates. It is important for patients to undergo thorough evaluation by an ENT specialist to exclude OSA and ensure appropriate surgical planning.Types of Snoring Surgery
Several surgical options exist to address non-OSA snoring. These include:- Uvulopalatopharyngoplasty (UPPP): Removal of excess tissue in the throat to widen the airway.
- Somnoplasty: A minimally invasive procedure using radiofrequency energy to shrink excess tissue in the palate and uvula.
- Laser-Assisted Uvulopalatoplasty (LAUP): Use of laser to remove parts of the uvula and soft palate.
- Pillar Procedure: Insertion of small implants into the soft palate to stiffen it and reduce vibration.
Effectiveness and Considerations
The effectiveness of surgical interventions for snoring varies, and evidence suggests that results can be mixed. Some individuals experience significant improvement, while others may have only minimal relief or require additional treatments. Factors influencing outcomes include the patient's overall health, anatomical characteristics, and adherence to postoperative care. Patients should be aware that surgery entails recovery time and potential complications, such as pain, infection, or changes in voice. Thorough consultation with healthcare providers, who will tailor advice based on individual circumstances, is essential for informed decision-making.Conclusion
In the UK, snoring surgery in the absence of OSA can offer relief for those unresponsive to conservative treatments. A range of surgical options is available, each with distinct risks and benefits. Individuals considering surgery should engage in detailed discussions with their healthcare providers to determine the most appropriate approach based on their specific needs and medical history. Always consult a specialist to explore all available evidence-based interventions before proceeding.Snoring Surgery Without Obstructive Sleep Apnoea (OSA)
What is Snoring?
Snoring means making noise when you breathe during sleep. It can be annoying and disturb sleep, both for the person who snores and their partner. If the snoring is not linked to Obstructive Sleep Apnoea (OSA), where breathing is not blocked badly, there are ways to help, like surgery.What is Non-OSA Snoring?
Non-OSA snoring is when parts of the throat, like the soft palate and uvula, vibrate and make noise, but there’s no big blockage like in OSA. Things like a blocked nose, being overweight, drinking alcohol, and how you sleep can make it worse. In the UK, non-OSA snoring is seen as both a health and a social issue because it affects sleep and relationships.Should You Think About Surgery for Snoring?
Think about surgery for snoring if changing habits and therapies like CPAP don’t work. If snoring makes life hard and these methods fail, surgery might help. A specialist doctor called an ENT should check everything and make sure surgery is right.Types of Snoring Surgeries
There are different surgeries to help with non-OSA snoring:- Uvulopalatopharyngoplasty (UPPP): Removes extra tissue in the throat to make space for air.
- Somnoplasty: Uses energy waves to shrink extra throat tissue.
- Laser-Assisted Uvulopalatoplasty (LAUP): Uses a laser to cut away parts of the soft palate and uvula.
- Pillar Procedure: Puts tiny supports in the soft palate to stop vibrations.
How Well Does Snoring Surgery Work?
Snoring surgery works differently for everyone. Some people feel much better, while others might need more help later. How well it works depends on your health, body, and if you follow doctor’s advice after. Remember, surgery needs time to heal and could lead to problems like pain, infection, or changes in voice. Talk a lot with your healthcare team, so you can choose what’s best for you.Conclusion
In the UK, snoring surgery, when there is no OSA, can help if other options don't work. There are different surgeries, each with risks and potential benefits. Before deciding, have detailed talks with your healthcare providers to find out what suits you best. Always check all the available options with a specialist.Frequently Asked Questions
What are evidence-based interventions for snoring surgery in the absence of Obstructive Sleep Apnea (OSA)?
Evidence-based interventions may include treatments such as uvulopalatopharyngoplasty (UPPP), laser-assisted uvulopalatoplasty (LAUP), and radiofrequency ablation among others.
Who is a candidate for snoring surgery without OSA?
Candidates are typically individuals who have significant social or personal complaints related to snoring but do not have diagnosed OSA.
What is uvulopalatopharyngoplasty (UPPP)?
UPPP is a surgical procedure that involves the removal of excess tissue from the throat to widen the airway and reduce snoring.
How effective is snoring surgery in the absence of OSA?
The effectiveness varies by individual, but studies have shown that many patients experience a reduction in snoring intensity and frequency post-surgery.
What are the risks associated with snoring surgery?
Risks can include pain, infection, swelling, changes in voice, and in rare cases, obstructive sleep apnea if not previously present.
Is snoring surgery covered by the NHS?
In the UK, snoring surgery is generally not covered by the NHS unless it is part of treatment for OSA. Most procedures would need to be funded privately.
What is the recovery time after snoring surgery?
Recovery time varies, but generally, patients can expect a recovery period of several days to a few weeks, depending on the specific procedure.
Can snoring return after surgery?
Yes, there is a possibility that snoring can return over time, especially if underlying factors such as weight gain or nasal congestion are not addressed.
Are there non-surgical alternatives to treating snoring?
Yes, non-surgical alternatives include lifestyle changes, CPAP therapy, dental appliances, positional therapy, and nasal strips or sprays.
What is laser-assisted uvulopalatoplasty (LAUP)?
LAUP is a procedure where a laser is used to remove or reshape the tissues in the throat (such as the uvula and soft palate) to reduce snoring.
How long does a snoring surgery procedure take?
Most snoring surgery procedures are relatively short, typically taking between 30 to 90 minutes depending on the complexity and specific method used.
Is radiofrequency ablation painful?
Radiofrequency ablation is generally considered less painful than traditional surgery, but patients may still experience some discomfort and soreness afterward.
What factors should I consider before opting for snoring surgery?
Consider the potential risks, effectiveness, cost, recovery time, and whether non-surgical alternatives have been tried and exhausted.
Do I need a referral to see a specialist for snoring surgery?
In the UK, you typically need a referral from your GP to see an ENT specialist for assessment and discussion of surgical options.
How should I prepare for snoring surgery?
Preparation may involve stopping certain medications, fasting for a period of time before the procedure, and arranging for post-surgery care and transportation.
What are good treatments for snoring without Obstructive Sleep Apnea (OSA)?
Some people snore but do not have Obstructive Sleep Apnea (OSA). Here are some treatments that can help:
- Surgery: Sometimes, a doctor can do surgery to help stop snoring.
- Special devices: Devices like nose strips or mouthpieces can be used to help breathe better.
- Position changes: Sleeping on your side can sometimes stop snoring.
- Healthy habits: Losing weight, not smoking, and avoiding alcohol before bed can help.
If you need help, you can ask a doctor or use simple tools like apps to track snoring. Remember, you can talk to someone you trust if you need more help.
There are different kinds of treatments that can help. Some of these are:
- Uvulopalatopharyngoplasty (UPPP): This is a type of surgery to help with breathing.
- Laser-assisted uvulopalatoplasty (LAUP): This uses a laser to help with breathing.
- Radiofrequency ablation: This uses radio waves to help with breathing.
If you're finding it hard to understand, you can ask a grown-up to help you. You can also use tools that read the text out loud, like text-to-speech apps.
Who can have snoring surgery if they do not have OSA?
Candidates are usually people who have big problems with snoring, but they do not have a sickness called OSA (which stands for Obstructive Sleep Apnea).
If you have trouble reading, it can help to:
- Read slowly and out loud.
- Use tools like audiobooks or text-to-speech apps.
- Ask someone to read with you and explain the parts you don't understand.
What is uvulopalatopharyngoplasty (UPPP)?
Uvulopalatopharyngoplasty, or UPPP, is a type of surgery.
The doctor does this surgery to help people who have problems with snoring or sleep apnea, which is when someone stops breathing for a short time while sleeping.
In the surgery, the doctor makes spaces in the throat bigger to help air move through better.
If you or someone you know needs to learn about this, ask a doctor for help, or you can watch videos or look at pictures that show how the surgery works.
UPPP is an operation. The doctor takes away extra tissue from your throat. This makes more space to help you breathe better and snore less.
Does snoring surgery work well if you do not have OSA?
Some people snore a lot. Sometimes, doctors do surgery to help. But, if you do not have OSA (a sleep problem), does the surgery help?
Here is what you can do:
- Talk to your doctor. They can tell you if surgery might help you.
- Use apps or tools that help with snoring. These can support your sleep.
- Try sleeping on your side. This can sometimes make snoring better.
Not everyone will have the same results, but doctors say a lot of people snore less and not as often after they have surgery.
What could go wrong with snoring surgery?
Things that might happen after can be:
- Pain
- Getting an infection
- Swelling (getting bigger)
- Changes in your voice
- Trouble breathing while you sleep (this is rare and only if it didn't happen before)
It’s good to talk to your doctor if you feel worried. They know how to help.
Does the NHS pay for snoring surgery?
Here is what you need to know:
- The NHS is the healthcare service in the UK.
- Sometimes, they pay for surgery if snoring causes serious health problems.
- Check with your doctor to see if you can have this help.
- Remember, doctors want to help, so ask them any questions you have.
Some tips to help you:
- Talk to your doctor or nurse if you are worried.
- Maybe take a friend or family member to help you understand.
- You can also write down questions to ask your doctor.
In the UK, the NHS usually does not pay for snoring surgery, unless it is to help treat a condition called OSA (Obstructive Sleep Apnea). Most of the time, you have to pay for these surgeries yourself.
How long does it take to get better after snoring surgery?
After you have surgery to help stop snoring, it will take some time to get better.
Most people start to feel a little better in a few days.
But it might take about 1 to 2 weeks to feel all better.
It is important to rest and follow the doctor’s advice.
If you get confused, you can ask someone to help you understand what the doctor said.
How long it takes to get better is different for everyone. Most people start to feel better after a few days or a few weeks. It depends on what kind of treatment they had.
Can snoring come back after an operation?
Snoring might come back after your throat or nose operation. Sometimes, the operation helps for a while, but snoring can return. If snoring comes back, it is important to talk to your doctor.
Here are some things that might help if snoring comes back:
- Try sleeping on your side instead of your back.
- Use a special pillow to keep your head up.
- Avoid alcohol before bed.
- Ask your doctor if a nasal strip could help.
If you have questions or worries, it's always best to talk to your doctor. They can help you understand and find a solution that works for you.
Yes, snoring can come back after some time. This can happen if things like putting on extra weight or having a stuffy nose are not taken care of.
Can you stop snoring without surgery?
Yes, there are other ways to help. You can make changes to how you live, use a special machine called CPAP, wear a mouthpiece, sleep in a different position, or use strips and sprays for your nose.
What is laser-assisted uvulopalatoplasty (LAUP)?
Laser-assisted uvulopalatoplasty, or LAUP, is a medical treatment that uses a laser to make the back of your throat bigger. This can help you breathe better, especially when you sleep.
Here are some tools or techniques that may help you understand better:
- Ask a doctor or nurse to explain it to you in person.
- Watch a simple video about LAUP.
- Use picture books that show how treatments like this work.
LAUP is a special way to help with snoring. A doctor uses a laser, which is a strong light, to change the shape of some parts inside the throat. These parts might be the uvula or the soft palate. This can help a person snore less.
If you find reading hard, here are some tips that can help:
- Use a ruler or your finger to follow the words.
- Ask someone to read it out loud with you.
- Try using audiobooks or text-to-speech programs to hear the information.
How long does surgery to stop snoring take?
Most snoring surgeries do not take long. They usually last between 30 minutes to 90 minutes. The time depends on how complicated the surgery is and which method is used.
Does radiofrequency ablation hurt?
Radiofrequency ablation usually hurts less than regular surgery. But people might feel a bit uncomfortable or sore after it.
What things should I think about before choosing snoring surgery?
Think about these things:
- What could go wrong?
- How well does it work?
- How much money does it cost?
- How long does it take to get better?
- Have you tried other ways that don't need surgery?
Do I need a referral to see a specialist for snoring surgery?
Do you need a note from your doctor to see a special doctor for snoring surgery?
If you are not sure, ask your doctor or your health helper. They can tell you what to do next.
You can also use tools like speaking to someone or drawings to help you understand. It is okay to ask for help.
In the UK, you usually need your doctor to tell you to see an ear, nose, and throat (ENT) specialist. The specialist will check you and talk about surgery choices.
Getting Ready for Snoring Surgery
Getting ready for the procedure might mean you need to stop taking some medicines, not eat for a while before, and plan for someone to take care of you and give you a ride home after the surgery.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Evidence-Based Interventions: snoring surgery in the absence of Obstructive Sleep Apnoea (OSA)
Relevance: 100%
-

Is snoring always a sign of sleep apnea?
Relevance: 89%
-

What is sleep apnea?
Relevance: 77%
-

What is sleep apnoea?
Relevance: 76%
-
What causes obstructive sleep apnea?
Relevance: 75%
-

How common is sleep apnea?
Relevance: 71%
-

What are the main types of sleep apnea?
Relevance: 71%
-

Does sleep apnea occur only in adults?
Relevance: 69%
-
What is complex sleep apnea syndrome?
Relevance: 67%
-
Introduction to obstructive sleep apnoea
Relevance: 66%
-

Is CPAP the only treatment for sleep apnea?
Relevance: 64%
-

Why is sleep apnea dangerous?
Relevance: 62%
-

What are common symptoms of sleep apnea?
Relevance: 62%
-
Can weight loss improve sleep apnea?
Relevance: 61%
-
What treatments are available for sleep apnea?
Relevance: 61%
-
How is sleep apnea diagnosed?
Relevance: 60%
-

What is complex sleep apnea syndrome?
Relevance: 60%
-

Can alcohol worsen sleep apnea?
Relevance: 59%
-

Can children have sleep apnea?
Relevance: 57%
-

Can sleep apnea be cured?
Relevance: 57%
-

What should I do if I suspect I have sleep apnea?
Relevance: 57%
-

What lifestyle changes can help manage sleep apnea?
Relevance: 52%
-

Am I eligible to try the new sleep apnea chip?
Relevance: 51%
-

What are risk factors for developing sleep apnea?
Relevance: 51%
-
How does the new Sleep Apnea Chip work?
Relevance: 46%
-

How does central sleep apnea differ from obstructive sleep apnea?
Relevance: 34%
-
Evidence-Based Interventions: tonsillectomy for recurrent tonsillitis surgery
Relevance: 32%
-

Weight Loss Surgery
Relevance: 29%
-
What is sleep apnoea?
Relevance: 26%
-

Is surgery necessary for Crohn's disease?
Relevance: 24%
-

What are the risks associated with baby sleep pillows?
Relevance: 23%
-

What is the safest sleep environment for an infant?
Relevance: 23%
-

Why are baby sleep pillows not safe for infants?
Relevance: 22%
-

Are baby sleep pillows safe?
Relevance: 22%
-

Prostate Surgery
Relevance: 21%
-

The Importance of Sleep for All Ages
Relevance: 21%
-

A journey to hip surgery
Relevance: 21%
-

Are there any benefits to using baby sleep pillows?
Relevance: 21%
-

How does sleep quality relate to menopause symptoms?
Relevance: 21%
-

Do crib wedges pose the same risks as baby sleep pillows?
Relevance: 20%


