Find Help
More Items From Ergsy search
-

Idiopathic pulmonary fibrosis (IPF) research
Relevance: 100%
-

What is Cystic Fibrosis?
Relevance: 37%
-

Pulmonary rehabilitation | NHS
Relevance: 32%
-

What is a pulmonary embolism?
Relevance: 30%
-

Sweat test | Diagnosing cystic fibrosis
Relevance: 29%
-

A guide to hospital-acquired deep vein thrombosis and pulmonary embolism
Relevance: 23%
-
Who can benefit from air physiotherapy?
Relevance: 16%
-

What research is being done on the Marburg virus?
Relevance: 16%
-

What research is being done on Huntington's disease?
Relevance: 16%
-

What research is being conducted on mosquito-borne diseases in the UK?
Relevance: 15%
-

What global organizations are involved in Nipah Virus research?
Relevance: 15%
-
Has research been conducted on the Nimbus variant?
Relevance: 15%
-

How significant is the reduction in funding for AIDS, Tuberculosis, and Malaria research?
Relevance: 14%
-

Epilepsy research: EEG | NHS
Relevance: 14%
-

Epilepsy research: EEG | NHS
Relevance: 14%
-

What type of research supports the role of diet in prostate cancer management?
Relevance: 14%
-
Where can I find research studies on air pollution and asthma in my area?
Relevance: 14%
-

Why is the UK cutting funding to AIDS, Tuberculosis, and Malaria research?
Relevance: 14%
-

Efforts to Combat Antibiotic Resistance Gain Momentum with New Research Initiatives
Relevance: 13%
-

Is online research sufficient to determine mis-selling?
Relevance: 13%
-

What further research is needed about menopause and dementia?
Relevance: 13%
-
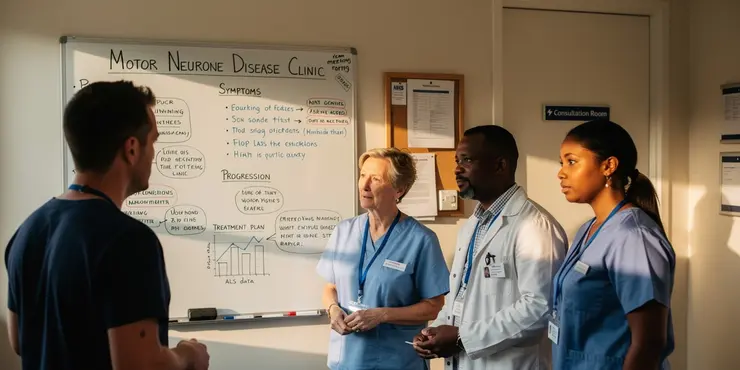
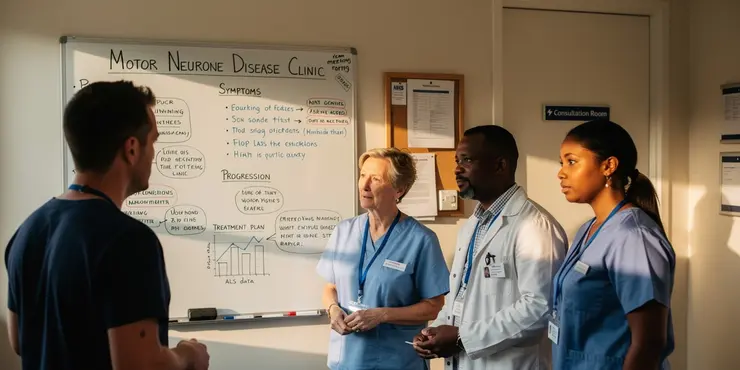
What research is being done on motor neurone disease?
Relevance: 12%
-
New Research Sheds Light on Long Covid Effects
Relevance: 12%
-

Are there any recent treatments or research developments for nut allergies?
Relevance: 12%
-

Is a prescription needed for air physiotherapy?
Relevance: 12%
-

Chest clearance techniques
Relevance: 11%
-

How does air physiotherapy work?
Relevance: 11%
-
COPD | NHS
Relevance: 11%
-
Is there research being done on mitochondrial disease?
Relevance: 11%
-

What are the types of thrombosis?
Relevance: 10%
-

Bronchiectasis class presentation v2
Relevance: 10%
-

Can air physiotherapy prevent respiratory infections?
Relevance: 10%
-
How to do the FIT bowel cancer screening test | Cancer Research UK
Relevance: 10%
-

How often should one perform air physiotherapy?
Relevance: 9%
-

What qualifications should a provider of air physiotherapy have?
Relevance: 9%
-

What equipment is used in air physiotherapy?
Relevance: 9%
-

Are there any exercises involved in air physiotherapy?
Relevance: 9%
-

How does PEP therapy work in air physiotherapy?
Relevance: 8%
-

What do researchers say about the link between paracetamol and autism?
Relevance: 8%
-

What are the reasons for the UK cutting funding to AIDS, Tuberculosis, and Malaria research?
Relevance: 8%
Idiopathic Pulmonary Fibrosis (IPF) Research in the United Kingdom
Understanding Idiopathic Pulmonary Fibrosis
Idiopathic Pulmonary Fibrosis (IPF) is a chronic, progressive lung disease characterized by the thickening and stiffening of tissue between the lung’s air sacs. This condition leads to a severe reduction in the ability to oxygenate blood, eventually causing significant respiratory complications. The term "idiopathic" indicates the unknown origin of the disease, making its precise causes largely enigmatic to the medical community.
Current Research Focus
In the United Kingdom, substantial efforts have been dedicated to uncovering the pathological mechanisms behind IPF. Leading institutions such as the National Institute for Health Research (NIHR) and the British Lung Foundation are heavily invested in studies elucidating genetic, environmental, and molecular facets of the disease. These studies aim to identify biological markers for early diagnosis and create new therapeutic approaches. Researchers are using cutting-edge techniques, including genomic sequencing and advanced imaging, to better understand disease progression.
Promising Treatment Advances
Recent trials in the UK have shown promise with antifibrotic medications such as pirfenidone and nintedanib. These drugs have been found to slow the progression of IPF, though they are not curative. Experimental therapies, including stem cell treatments and gene editing technologies like CRISPR, are also under investigation. The goal is to not only halt disease progression but potentially reverse the fibrosis, bringing hope to patients affected by IPF.
Patient Involvement in Research
Another significant aspect of IPF research in the UK is patient involvement. Patients and their families are increasingly included in clinical trials and study designs, ensuring that research outcomes are directly relevant to those living with the disease. Organizations such as Action for Pulmonary Fibrosis provide crucial platforms for patient advocacy and education, bridging the gap between researchers and the community.
Future Directions and Challenges
The future of IPF research in the UK holds promise but also faces several challenges. Ensuring widespread access to innovative treatments and maintaining funding for expansive research are critical hurdles. Collaboration between public health entities, private organizations, and academic institutions will be paramount in driving forward the understanding and treatment of IPF.
With continued efforts and support, the research community in the UK aims to transform IPF from a terminal diagnosis to a manageable condition, improving the quality of life for countless individuals.
Idiopathic Pulmonary Fibrosis (IPF) Research in the United Kingdom
What is Idiopathic Pulmonary Fibrosis?
Idiopathic Pulmonary Fibrosis, or IPF, is a lung disease. It makes the lung tissue thick and hard. This makes it hard to breathe. The word "idiopathic" means doctors don't know what causes it.
What Are Scientists Studying?
In the UK, scientists are trying to learn more about IPF. Big groups like the National Institute for Health Research (NIHR) and the British Lung Foundation are helping. They want to understand what causes IPF. They are looking at genes and the environment. They use special tools to study the lungs. This can help find the disease early and make new medicines.
New Medicines and Treatments
Medicines like pirfenidone and nintedanib can slow down IPF. But they do not cure it. Scientists are also looking at new ideas like using stem cells and gene editing to help the lungs get better. This gives hope to people with IPF.
Patients Helping with Research
In the UK, people with IPF and their families are helping with research. They join trials and share their experiences. Groups like Action for Pulmonary Fibrosis give patients a voice and help them learn more.
What's Next for Research?
Research in the UK is making progress, but there are challenges. It's important to make sure new treatments are available to everyone. More money and support are needed. Many groups need to work together to help people with IPF.
With teamwork and continued research, experts hope to turn IPF into a condition that can be managed. This will help people live better lives.
Frequently Asked Questions
What is idiopathic pulmonary fibrosis (IPF)?
Idiopathic pulmonary fibrosis (IPF) is a chronic and progressive lung disease characterized by the thickening and scarring (fibrosis) of lung tissue without a known cause.
What are the common symptoms of IPF?
Common symptoms of IPF include shortness of breath, a persistent dry cough, fatigue, unexplained weight loss, and clubbing (widening and rounding) of the fingertips or toes.
How is IPF diagnosed?
IPF is diagnosed through a combination of clinical evaluation, lung function tests, high-resolution CT scans, and sometimes a lung biopsy to rule out other conditions.
What causes IPF?
The exact cause of idiopathic pulmonary fibrosis is unknown, hence the term 'idiopathic.' However, genetic and environmental factors, such as smoking and exposure to certain dusts, may play a role.
Is there a cure for IPF?
Currently, there is no cure for IPF. Treatment focuses on managing symptoms and slowing disease progression through medications, pulmonary rehabilitation, and sometimes lung transplantation.
What medications are used to treat IPF?
Two antifibrotic medications, nintedanib and pirfenidone, are commonly used to slow the progression of IPF. Other treatments may include oxygen therapy and medications to manage symptoms.
Can lifestyle changes help manage IPF?
Yes, lifestyle changes such as quitting smoking, eating a balanced diet, staying active, and managing stress can help improve overall health and quality of life for individuals with IPF.
What support is available for people with IPF in the UK?
Support for people with IPF in the UK includes specialist respiratory care teams, support groups, charities like Action for Pulmonary Fibrosis, and financial aid for necessary treatments.
How does pulmonary rehabilitation help IPF patients?
Pulmonary rehabilitation helps IPF patients by providing exercise training, education, and support to improve physical fitness, reduce symptoms, and enhance overall quality of life.
What are the risk factors for developing IPF?
Risk factors for developing IPF include age (usually affects people over 50), a family history of IPF, smoking, and occupational exposure to certain dusts and pollutants.
Can IPF be prevented?
There is no known prevention for IPF, but reducing risk factors such as avoiding smoking and harmful exposures may lower the likelihood of developing the disease.
How does IPF affect life expectancy?
IPF significantly impacts life expectancy, with average survival from diagnosis ranging from 3 to 5 years, though this can vary widely depending on individual circumstances and treatment response.
What is the role of a multidisciplinary team in managing IPF?
A multidisciplinary team, including physicians, nurses, physiotherapists, and social workers, collaborates to provide comprehensive care, manage symptoms, and support IPF patients and their families.
What research is being done on IPF?
Ongoing research on IPF includes studying the disease's underlying mechanisms, developing new treatments, and conducting clinical trials to find more effective therapies.
How can I participate in IPF research or clinical trials?
To participate in IPF research or clinical trials, you can speak with your healthcare provider, check with specialist IPF centres, or visit the UK Clinical Trials Gateway for information on current studies.
What is idiopathic pulmonary fibrosis (IPF)?
Idiopathic pulmonary fibrosis, or IPF, is a lung disease. It makes it hard to breathe. In IPF, the lungs get thick and stiff.
Doctors do not know what causes IPF. "Idiopathic" means we do not know the cause.
If you have trouble reading, try using tools like audiobooks or text-to-speech apps that can read text out loud to you.
Idiopathic pulmonary fibrosis (IPF) is a long-lasting lung sickness. It makes the lungs get thicker and scarred. We do not know what causes it.
What signs show you might have IPF?
IPF stands for Idiopathic Pulmonary Fibrosis. It is a lung illness. Here are some signs that mean you might have IPF:
- Feeling out of breath even when you do simple things.
- Getting a new cough that does not go away.
- Feeling very tired all the time.
- Losing weight without trying.
- A crackling sound in your chest when you breathe.
If you feel these things, it is a good idea to see a doctor. They can help you feel better.
Tools to help:
- Use a diary to note down when you feel these signs.
- Bring someone with you to the doctor to help remember things.
Some signs of IPF are:
- Feeling short of breath
- Having a dry cough that doesn't go away
- Feeling very tired
- Losing weight without trying
- Fingertips or toes getting wider and rounder
If you have trouble reading, you can try:
- Listening to audiobooks
- Using text-to-speech tools
- Asking someone to read it to you
How do doctors find out if someone has IPF?
Doctors use different tests to see if a person has IPF.
They may ask for a scan to look at the lungs.
Doctors might listen to the lungs by using a stethoscope.
They could also do a breathing test to check how well the lungs work.
Sometimes, a small part of the lung might be taken out to look at it closely. This is called a biopsy.
Using simple words and clear pictures can help you understand what will happen when doctors test you for IPF.
If you find any of the words or steps hard, ask a doctor or nurse to explain them to you.
Doctors find out if someone has IPF by doing several things. They talk to the person and check their health. They do tests to see how well their lungs work. They take special pictures of the lungs called high-resolution CT scans. Sometimes, they need to take a tiny piece of the lung, called a biopsy, to make sure it's not something else.
Tools like pictures, notes, and simple explanations can help understand this better. Asking questions and using reading help, like audiobooks, can also be useful.
What makes IPF happen?
Doctors do not know exactly why IPF happens. It might be caused by breathing in bad things like dust or smoke. Some people might have genes from their family that make them get sick easier.
If you find reading hard, try using pictures or videos to learn more. You can also ask someone to read with you or use an app that reads the text out loud.
We don't know exactly what causes idiopathic pulmonary fibrosis. That's why we call it 'idiopathic.' But things like your genes and the environment might be part of the cause. Smoking or being around certain kinds of dust might make it happen.
Can IPF be fixed?
Doctors cannot fully fix IPF right now. But there are things that can help:
- Medicines: Some medicines can make you feel better and slow down IPF.
- Breathing Help: You can use oxygen to help you breathe easier.
- Healthy Living: Eating healthy food and staying active can help you feel better.
- Doctor Visits: Go to the doctor often to check your lungs.
Having support from family and friends can also make a big difference. Use simple reminders and ask for help when you need it.
Right now, there is no way to cure IPF. Doctors can help make it better by giving medicine, special exercises to help you breathe, and sometimes giving a new lung if needed.
What medicines help with IPF?
IPF means your lungs are sick. Doctors give medicine to help.
- Some pills help your lungs stay strong.
- Other pills help you breathe better.
Ask your doctor which pills are best for you.
Using pictures or videos can help you understand better.
Two medicines called nintedanib and pirfenidone can help slow down a sickness in the lungs called IPF. Other ways to help might be using oxygen or other medicines to feel better.
Can changing how I live help with my IPF?
Yes, you can feel better if you make some changes in how you live. Stop smoking, eat good food, move your body, and try to stay calm. This can help you feel healthier and happier, even if you have a condition like IPF.
Here are some tips to help:
- Ask a doctor or nurse for help if you want to stop smoking.
- Try eating fruits, veggies, and whole grains.
- Find fun ways to exercise, like walking or dancing.
- Learn ways to relax, like deep breathing or listening to music.
What help can people with IPF get in the UK?
People with IPF can get different types of help in the UK. Here are some ideas:
- Doctors and Nurses: You can see doctors and nurses who know a lot about IPF. They help you feel better.
- Medicines: There are medicines that can help slow down IPF. Your doctor can tell you about them.
- Support Groups: Joining a support group can be good. You can talk to other people with IPF who understand.
- Breathing Exercises: Doing special breathing exercises can make your lungs stronger. A therapist can show you how.
- Visit Your GP: Your GP can give you advice about the help you need.
It is important to talk to a doctor about the best help for you.
In the UK, people with IPF can get help from special breathing care teams. There are support groups where people can talk and share. Charities like Action for Pulmonary Fibrosis give help too. People can also get money to pay for treatments they need.
How can exercise help people with lung problems?
Exercise programs, like lung rehab, can help people who have breathing problems. They help people feel better and have more energy. Here’s how:
- Help with breathing exercises: Breathing exercises make your lungs stronger.
- Making muscles stronger: Exercise helps your body stay strong.
- Teaching ways to breathe better: Learn how to breathe easier.
- Getting help from doctors and therapists: They help you learn and get better.
Using easy tools can help too:
- Listening to calm music while you exercise.
- Using simple apps that remind you to breathe deep.
- Joining a group to have fun and talk to others.
Pulmonary rehabilitation is a program that helps people with IPF, a lung problem. It includes exercise to get stronger, learning sessions, and support. This program helps you feel better, have fewer symptoms, and enjoy life more.
What makes it more likely to get IPF?
Here are some things that might make you more likely to get IPF:
- Being older
- Being a man
- Smoking
- Working with dust or fumes
- Having family members with lung problems
If you are worried, it helps to talk to a doctor. They can give good advice. You can also use apps or videos that explain things slowly and clearly.
Things that can make someone more likely to get IPF:
- Getting older - It usually happens to people over 50.
- Having family members with IPF - if it runs in the family.
- Smoking - Breathing in smoke from cigarettes.
- Being around certain dust or bad air at work.
If reading is hard, try these:
- Use a ruler or finger to follow the words.
- Read out loud with someone.
- Take breaks often.
Can IPF Be Stopped?
IPF means a problem with the lungs. It makes it hard to breathe.
Right now, there is no way to stop IPF from happening. But you can make it better. Here are some things that help:
- Don’t smoke. Smoking can hurt your lungs more.
- Take medicine your doctor gives you. It can help you feel better.
- Do breathing exercises. A doctor or therapist can teach you these.
- Use oxygen if your doctor says you need it. It can help you breathe.
- Eat healthy food and get plenty of rest.
If you or someone you know has trouble reading, ask a friend or family member for help. You can also listen to an audiobook or use a reading tool that reads aloud.
We can't stop IPF from happening for sure. But there are things you can do to help. Not smoking and staying away from things that can hurt your lungs may help you not get this disease.
How does IPF affect life expectancy?
IPF is short for Idiopathic Pulmonary Fibrosis. It is a lung disease.
People with IPF have scarring in their lungs. This makes it hard to breathe.
IPF can change how long a person lives. This is called life expectancy.
People with IPF may need to visit the doctor often. They may also need medicine or special help to breathe.
Doctors can help people with IPF manage their symptoms. This means they can feel better and be more comfortable.
It is important to talk to a doctor about IPF. The doctor can explain more and give support.
Good tools: Use pictures or videos to help understand more about IPF. Bring someone with you to the doctor to help listen and ask questions.
IPF is a lung disease. It can make life shorter. On average, people live about 3 to 5 more years after doctors find it. But, this time can be different for each person. It depends on how their body reacts to treatment and other personal factors.
What does a team of different helpers do to take care of IPF?
Sometimes people have a lung illness called IPF. It makes it hard to breathe. To help, doctors and other helpers work together.
This team has different people like:
- Doctors - They check your health and give medicine.
- Nurses - They take care of you and help you understand your treatment.
- Therapists - They help you breathe better.
Each person in the team helps in different ways. They talk to each other and work together to help you feel better.
If you need help understanding, you can:
- Ask someone to explain things step by step.
- Use pictures to help understand.
- Ask for things to be repeated if needed.
A group of different helpers like doctors, nurses, exercise helpers, and social workers work together. They take care of people with IPF and help their families too. They make sure everyone feels better and has all the support they need.
What Research Is Being Done on IPF?
Scientists are working hard to understand IPF (Idiopathic Pulmonary Fibrosis). IPF is a disease that makes it hard to breathe.
They ask questions like:
- Why do people get IPF?
- How can we help people with IPF feel better?
Doctors and scientists do tests to find new medicines. They want to help people with IPF live longer and feel healthier.
If reading is hard, you can:
- Ask someone to read this to you.
- Use a computer program that reads text out loud.
Scientists are learning more about a disease called IPF. They are trying to understand why it happens, find new medicines, and test these to see if they work better.
Here are some ways to help you understand this information:
- Use a dictionary to look up hard words.
- Ask someone to explain the tough parts.
- Take breaks if it feels like a lot to read.
How can I join IPF research or clinical trials?
If you want to help in IPF studies or trials, you can. IPF is a lung illness. Doctors and scientists do studies to learn more and find treatments. Here is how you can help:
1. Talk to Your Doctor: Ask your doctor if there are studies or trials you can join.
2. Search Online: Look for websites that list trials. You can try ClinicalTrials.gov. Type "IPF" to find trials near you.
3. Join a Patient Group: Some groups have info on studies. They can tell you how to join.
Helpful Tools:
- Ask for Help: If reading is hard, ask someone to help read and explain.
- Use Apps: Some apps read text out loud. Try them if they help you understand better.
If you decide to join, the doctors will explain everything. You can ask questions any time!
If you want to help with IPF research or tests, you can:
- Talk to your doctor.
- Look at special IPF centers.
- Visit the UK Clinical Trials Gateway to find studies happening now.
These steps can help you find ways to join in. It's good to ask someone for help if needed. You can also use tools like screen readers or reading apps to make it easier to read.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Idiopathic pulmonary fibrosis (IPF) research
Relevance: 100%
-

What is Cystic Fibrosis?
Relevance: 37%
-

Pulmonary rehabilitation | NHS
Relevance: 32%
-

What is a pulmonary embolism?
Relevance: 30%
-

Sweat test | Diagnosing cystic fibrosis
Relevance: 29%
-

A guide to hospital-acquired deep vein thrombosis and pulmonary embolism
Relevance: 23%
-
Who can benefit from air physiotherapy?
Relevance: 16%
-

What research is being done on the Marburg virus?
Relevance: 16%
-

What research is being done on Huntington's disease?
Relevance: 16%
-

What research is being conducted on mosquito-borne diseases in the UK?
Relevance: 15%
-

What global organizations are involved in Nipah Virus research?
Relevance: 15%
-
Has research been conducted on the Nimbus variant?
Relevance: 15%
-

How significant is the reduction in funding for AIDS, Tuberculosis, and Malaria research?
Relevance: 14%
-

Epilepsy research: EEG | NHS
Relevance: 14%
-

Epilepsy research: EEG | NHS
Relevance: 14%
-

What type of research supports the role of diet in prostate cancer management?
Relevance: 14%
-
Where can I find research studies on air pollution and asthma in my area?
Relevance: 14%
-

Why is the UK cutting funding to AIDS, Tuberculosis, and Malaria research?
Relevance: 14%
-

Efforts to Combat Antibiotic Resistance Gain Momentum with New Research Initiatives
Relevance: 13%
-

Is online research sufficient to determine mis-selling?
Relevance: 13%
-

What further research is needed about menopause and dementia?
Relevance: 13%
-
What research is being done on motor neurone disease?
Relevance: 12%
-
New Research Sheds Light on Long Covid Effects
Relevance: 12%
-

Are there any recent treatments or research developments for nut allergies?
Relevance: 12%
-

Is a prescription needed for air physiotherapy?
Relevance: 12%
-

Chest clearance techniques
Relevance: 11%
-

How does air physiotherapy work?
Relevance: 11%
-
COPD | NHS
Relevance: 11%
-
Is there research being done on mitochondrial disease?
Relevance: 11%
-

What are the types of thrombosis?
Relevance: 10%
-

Bronchiectasis class presentation v2
Relevance: 10%
-

Can air physiotherapy prevent respiratory infections?
Relevance: 10%
-
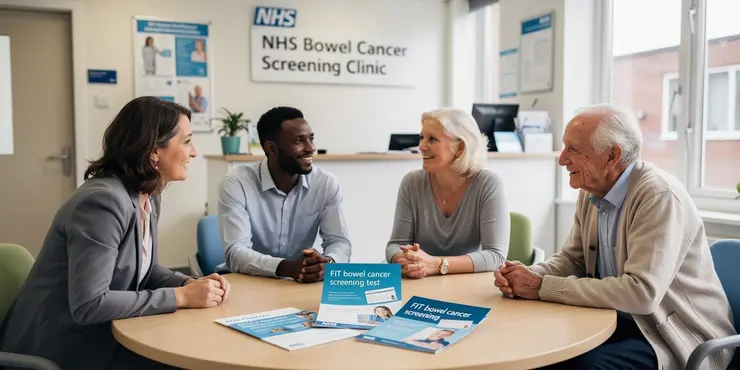
How to do the FIT bowel cancer screening test | Cancer Research UK
Relevance: 10%
-

How often should one perform air physiotherapy?
Relevance: 9%
-

What qualifications should a provider of air physiotherapy have?
Relevance: 9%
-

What equipment is used in air physiotherapy?
Relevance: 9%
-

Are there any exercises involved in air physiotherapy?
Relevance: 9%
-

How does PEP therapy work in air physiotherapy?
Relevance: 8%
-

What do researchers say about the link between paracetamol and autism?
Relevance: 8%
-

What are the reasons for the UK cutting funding to AIDS, Tuberculosis, and Malaria research?
Relevance: 8%


