Find Help
More Items From Ergsy search
-

Evidence-Based Interventions: haemorrhoid surgery
Relevance: 100%
-
What can I do about haemorrhoids? | NHS
Relevance: 93%
-

Bleeding from the bottom rectal bleeding
Relevance: 41%
-
Bleeding from the bottom rectal bleeding
Relevance: 35%
-

What are the benefits of insoluble fiber?
Relevance: 30%
-

How does fiber benefit digestion?
Relevance: 26%
-

How does fiber benefit digestion?
Relevance: 20%
-

What is a fecal occult blood test?
Relevance: 19%
-

Can too much fiber be harmful?
Relevance: 15%
-

What are the symptoms of BPH?
Relevance: 14%
-

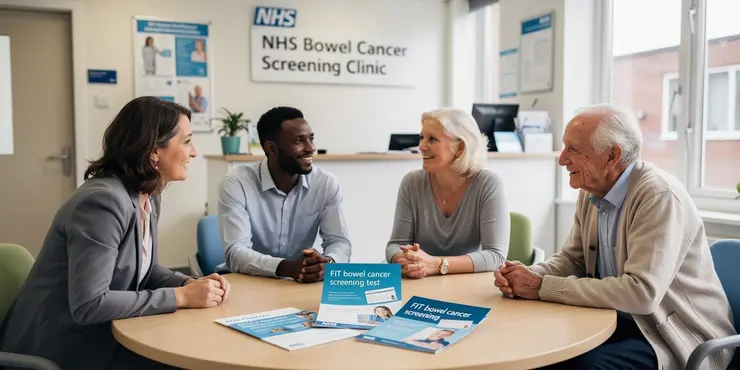
How to use the bowel cancer screening FIT kit | NHS
Relevance: 14%
-

What is Bowel Cancer?
Relevance: 14%
-

Is a colonoscopy necessary after a positive home test?
Relevance: 14%
-

How does a fecal occult blood test (FOBT) work?
Relevance: 12%
-
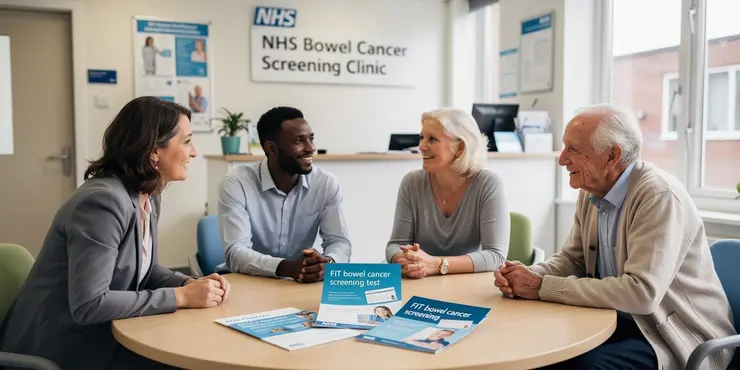
How to do the FIT bowel cancer screening test | Cancer Research UK
Relevance: 6%
-

How to treat constipation | NHS
Relevance: 6%
-

Is fibre good for health?
Relevance: 6%
-

Why is fiber important for gut health and aging?
Relevance: 6%
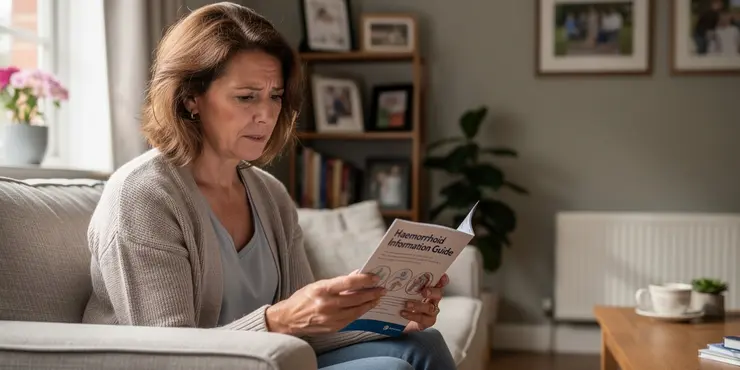
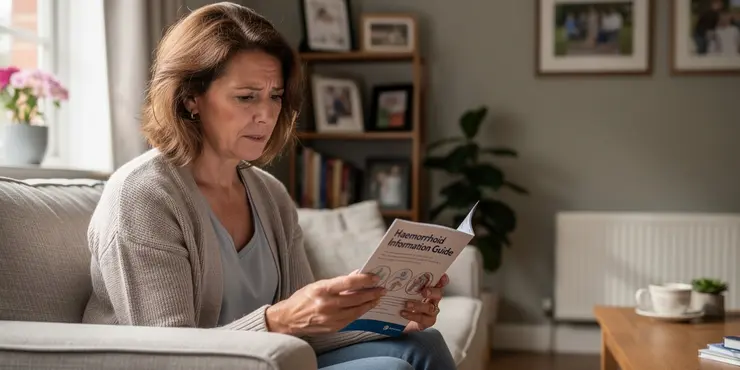
What Can I Do About Haemorrhoids? | NHS
Understanding Haemorrhoids
Haemorrhoids, also known as piles, are swollen blood vessels found inside or around the bottom (the rectum and anus). They are a common condition and can cause discomfort, itching, pain, and bleeding. In the UK, haemorrhoids affect around 4.4% of the population and are more common in adults aged 45-65.Symptoms of Haemorrhoids
Some of the common symptoms include:- Bleeding after passing a stool – the blood is usually bright red.
- Itchy bottom.
- A lump hanging outside the anus, which may need to be pushed back in after passing a stool.
- A mucus discharge after passing a stool.
- Soreness, redness, and swelling around your anus.
Home Treatments and Lifestyle Changes
For most people, haemorrhoids improve within a few days without requiring treatment. Here are some things you can do at home to help ease the discomfort:- Increase Fibre Intake: Eating high-fibre foods like fruits, vegetables, and whole grains can ease the passage of stools and reduce the strain that may cause haemorrhoids.
- Stay Hydrated: Drinking plenty of water helps to keep stools soft.
- Avoid Straining: Try not to strain when on the toilet, as this can exacerbate haemorrhoids.
- Regular Exercise: Engaging in regular physical activity can help prevent constipation and reduce pressure on veins.
- Warm Sitz Baths: Soaking the anal area in warm water for 10-15 minutes several times a day can provide relief.
Over-the-Counter Treatments
Pharmacies in the UK offer various over-the-counter treatments to relieve haemorrhoid symptoms. These include:- Creams and Ointments: Products containing hydrocortisone help reduce inflammation and itching.
- Suppositories: Inserted into the rectum to treat internal piles, these can help alleviate pain and swelling.
- Cold Packs: Applying a cold pack can reduce swelling and provide pain relief.
When to See a GP
While haemorrhoids often improve with home treatments, you should see your GP if you experience:- Persistent or severe pain.
- Continuous bleeding or bright red blood in your stool.
- No improvement after seven days of home treatment.
Conclusion
Haemorrhoids can be uncomfortable, but they are generally manageable with self-care and over-the-counter treatments. By making lifestyle changes and seeking medical advice when necessary, most people can find relief from their symptoms. If you are concerned about your symptoms or if they persist, do not hesitate to contact your GP for further guidance.What Can I Do About Haemorrhoids? | NHS
Understanding Haemorrhoids
Haemorrhoids, also called piles, are swollen blood vessels. They are inside or around your bottom (rectum and anus). Many people have them. They can make you feel itchy, sore, and cause bleeding. In the UK, about 4 out of 100 people have haemorrhoids, mostly adults aged 45-65.Symptoms of Haemorrhoids
How to tell if you have haemorrhoids:- Bleeding after you go to the toilet – the blood is bright red.
- Itchy bottom.
- A lump outside your bottom that you may need to push back in.
- Mucus on toilet paper after wiping.
- Sore, red, and swollen area around your bottom.
Home Treatments and Lifestyle Changes
Most haemorrhoids get better on their own in a few days. Here are things you can do at home to feel better:- Eat More Fibre: Foods like fruits, vegetables, and whole grains help make stools softer and easier to pass.
- Drink Water: Keep hydrated to help keep stools soft.
- Don’t Strain: Try not to push too hard when on the toilet.
- Exercise Regularly: Moving around can help stop constipation and reduce vein pressure.
- Take Warm Baths: Soak your bottom in warm water for 10-15 minutes a few times a day to feel better.
Over-the-Counter Treatments
You can get medicines from the pharmacy to relieve haemorrhoids:- Creams and Ointments: Some contain hydrocortisone to reduce swelling and itching.
- Suppositories: These are placed inside your bottom to help with pain and swelling.
- Cold Packs: Using a cold pack can make swelling go down and ease pain.
When to See a GP
Most times, haemorrhoids improve on their own. But see your doctor if:- You have bad pain that doesn’t go away.
- You see bright red blood in your stool often.
- You haven’t gotten better after using home treatments for seven days.
Conclusion
Haemorrhoids can be uncomfortable, but you can often manage them with self-care and pharmacy treatments. By changing your lifestyle and getting medical advice, most people find relief. If your symptoms bother you or don’t go away, talk to your doctor.Frequently Asked Questions
What are haemorrhoids?
Haemorrhoids, also known as piles, are swellings containing enlarged blood vessels found inside or around the bottom (the rectum and anus).
What are the common symptoms of haemorrhoids?
Common symptoms include bleeding after passing a stool, itchy bottom, a lump hanging outside the anus that may need to be pushed back in after passing a stool, and a mucus discharge after passing a stool.
What causes haemorrhoids?
The exact cause is unclear, but they are often associated with increased pressure in the blood vessels in and around the anus. Contributing factors include chronic constipation or diarrhoea, straining during bowel movements, pregnancy, and ageing.
How can I prevent haemorrhoids?
To prevent haemorrhoids, maintain a high-fibre diet to keep stools soft, drink plenty of fluids, avoid straining during bowel movements, and exercise regularly.
When should I see a GP for haemorrhoids?
See a GP if you experience bleeding from the bottom, if over-the-counter treatments haven't helped, or if you continue to have symptoms like severe pain or discomfort.
What over-the-counter treatments are available for haemorrhoids?
Over-the-counter treatments include creams, ointments, and suppositories, which can help to reduce swelling and discomfort.
Are there any home remedies for haemorrhoids?
Home remedies include soaking in a warm bath several times a day, especially after bowel movements, and using moist wipes instead of dry toilet paper.
Can lifestyle changes help manage haemorrhoids?
Yes, lifestyle changes like increasing dietary fibre intake, staying hydrated, and avoiding prolonged sitting on the toilet can help manage and prevent haemorrhoids.
Can haemorrhoids go away on their own?
Small haemorrhoids can sometimes improve on their own without treatment. However, lifestyle changes and over-the-counter treatments can help relieve symptoms more quickly.
Are haemorrhoids dangerous?
Haemorrhoids are not usually dangerous, but they can be extremely uncomfortable. Persistent or severe cases should be evaluated by a healthcare provider.
What medical procedures are available for severe haemorrhoids?
For more severe haemorrhoids, treatments include banding (where a tight elastic band is placed around the base of the haemorrhoid to cut off its blood supply), sclerotherapy (where a hardening agent is injected to shrink the haemorrhoid), and surgical removal.
Can I exercise with haemorrhoids?
Yes, gentle exercise such as walking can help stimulate bowel function. However, avoid heavy lifting or strenuous activities that could exacerbate the haemorrhoids.
Is it safe to use pain relievers for haemorrhoid pain?
Over-the-counter pain relievers such as paracetamol can be used to alleviate pain. Follow the dosage instructions and consult a healthcare provider if you are unsure.
What should I eat to help with haemorrhoids?
A diet high in fibre, including fruits, vegetables, whole grains, and legumes, can help produce soft stools that are easier to pass and reduce the risk of haemorrhoids.
Can sitting for long periods cause haemorrhoids?
Yes, sitting for extended periods, particularly on the toilet, can contribute to the development of haemorrhoids by increasing pressure on the blood vessels in the anal area.
What are piles?
Piles are swollen lumps inside or around your bottom. They can be itchy or sore. Sometimes, they can bleed when you poo.
If piles hurt or bleed a lot, tell a grown-up or someone who helps you. They can get a doctor to help.
To feel better:
- Try not to push too hard when you go to the toilet.
- Eat lots of fruits and veggies to help you poo more easily.
- Drink plenty of water.
If reading is tricky, you can ask someone to read this with you.
Piles are also called haemorrhoids. They are lumps with big blood vessels. You can find them inside or around your bottom (the rectum and anus).
If you have trouble reading, you can ask someone to read it to you. You can also use reading tools that read the text out loud.
What are the common signs of piles?
Here are some signs you might notice:
- Bleeding after you go to the toilet.
- An itchy feeling around your bottom.
- A lump that sticks out from your bottom. You might need to push it back in after going to the toilet.
- A slimy liquid coming out of your bottom after you go to the toilet.
To help remember or understand these signs, you can:
- Use picture cards to match words with images.
- Ask someone to read with you and explain the signs.
- Use simple drawings to help visualize each symptom.
What makes piles happen?
Piles are lumps or bumps near your bottom. They might hurt or itch. Here are some things that can make piles happen: - Too much pushing when you poo. - Sitting on the toilet for a long time. - Not eating enough fruits and veggies. These help you poo easily. - Lifting heavy things often. - Being very overweight. To make it better, you can: - Eat foods with lots of fiber, like fruits and vegetables. - Drink lots of water. - Exercise a little every day. If it still hurts, you can tell an adult or a doctor. They can help you.The exact cause is unclear, but they are often related to pressure in the blood vessels in and around the anus. Contributing factors include chronic constipation or diarrhoea, straining during bowel movements, pregnancy, and ageing.
How can I stop getting piles?
To stop haemorrhoids, eat food with lots of fibre to help make poo soft. Drink lots of water. Don’t push too hard when you go to the toilet. Exercise often.
When should I see a doctor for piles?
Piles are sore bumps in your bottom. They can be itchy and hurt.
See a doctor if:
- You have piles for more than a week.
- Piles are very painful or bleed a lot.
- You feel worried or not sure about your piles.
Here are some helpful things:
- Ask a friend or family member to go with you to the doctor.
- Write down your questions and take them to your appointment.
- You can draw or use pictures to show how you feel.
Go to the doctor if you see blood when you go to the toilet. Also, visit the doctor if medicine from the shop doesn't help or if you still have a lot of pain or feel very uncomfortable.
It might help to talk to someone you trust about how you feel. Writing down your symptoms can help you remember when you talk to the doctor.
What medicines can I buy to help with piles?
Piles are swollen bumps in your bottom that can hurt. You can buy some medicines from the shop to help with piles.
Here are some things that can help:
- Creams or ointments: Put this on the sore area to help stop pain and itching.
- Suppositories: These are small things you put gently into your bottom. They can help with swelling and pain.
- Painkillers: You can take pills like paracetamol to help with pain.
Ask a grown-up or someone at the pharmacy to help you pick the right one. They are good at helping with this.
You can buy some medicines without a doctor's note. These can be creams, ointments, or special pills you put in your bottom. They help make the swelling go down and stop it from hurting.
If you find reading hard, you can use tools to help. You can try listening to audiobooks or using screen readers on computers and phones. These can read the words out loud to you. You can also ask someone you trust to help you read or understand this. Using bright colors to highlight important words or drawing pictures can also make things clearer.
Can you treat piles at home?
Here are some ways to feel better at home:
You can sit in a warm bath a few times each day. It's a good idea to do this after using the bathroom.
Try using wet wipes instead of dry toilet paper. Wet wipes can be softer on your skin.
If you need help reading, you can ask someone to read it with you, or use an app that reads out loud. You can also look at pictures or videos about this topic online.
Can changing how I live help with piles?
Yes, changing some things in your life can help with piles (haemorrhoids). You can eat more foods with fibre, drink lots of water, and not sit on the toilet for too long.
Do piles go away by themselves?
Piles are little lumps near your bottom. Sometimes they hurt or bleed.
Piles can get better without help. Eating healthy food, like fruits and vegetables, can help. Drinking lots of water is good too. Try not to sit for too long.
If piles do not get better, seeing a doctor can help.
Helpful tip: Use cushions when sitting to feel more comfortable.
Small piles can get better without help. But, changing some everyday habits and using medicine from the shop can make you feel better faster.
Are piles dangerous?
Piles are lumps inside or around your bottom. They are not usually dangerous.
If piles hurt or bleed, see a doctor to get help.
Tools like picture books can help you understand more about piles.
Haemorrhoids are not usually dangerous, but they can be very uncomfortable. If they don't go away or are really bad, you should see a doctor.
What can doctors do for bad haemorrhoids?
If you have bad haemorrhoids, doctors can help in different ways. They might do small surgeries to make you feel better.
Here are some things doctors can do:
- Banding: Doctors put a tiny band around the haemorrhoid to make it smaller.
- Injection: Doctors use a needle to put medicine into the haemorrhoid to shrink it.
- Laser treatment: A special light is used to make the haemorrhoid go away.
- Surgery: If the haemorrhoid is very bad, doctors might need to remove it with surgery.
If you need help reading, you can ask someone to read with you, use special apps to read aloud, or use audio books to get more information.
If piles are bad, doctors can help in different ways. They can use a small rubber band. This band goes around the pile to stop blood from getting to it. This helps the pile go away. Another way is by using a special medicine. The medicine makes the pile shrink. Sometimes, doctors need to remove the pile with surgery.
Can I exercise if I have haemorrhoids?
It's okay to do some exercise if you have haemorrhoids, but be gentle and careful. Listen to your body and stop if it hurts.
Try to choose activities that are not too hard, like walking or swimming. These are good and gentle exercises.
If you feel any pain or are not sure what to do, it is important to talk to a doctor. They can help you know what is safe.
Using a cushion when sitting can make you feel more comfortable. Remember to drink lots of water and eat foods with lots of fiber. This helps to make going to the bathroom easier and can help with the pain.
Yes, doing gentle exercise like walking can help make your tummy work better. But do not lift heavy things or do hard exercise because this can make piles worse.
Can you safely use pain medicine for haemorrhoid pain?
When you have haemorrhoid pain, you might want to use medicine to feel better. It is important to check with a doctor or nurse first. They will tell you what medicine is safe to use.
Here are some tips to help:
- Ask a doctor or pharmacist for advice.
- Read the medicine box to know how much to take.
- If you still have pain, talk to your doctor again.
Remember, always make sure the medicine is safe for you!
You can take medicine like paracetamol to help with pain. Make sure to follow the instructions on the packet. If you are not sure what to do, ask a doctor or nurse for help.
What foods can help if I have piles?
Eating foods with lots of fibre can help. This includes fruits, vegetables, whole grains, and beans. These foods make it easier to go to the toilet and help stop piles from forming.
Can sitting for a long time cause piles?
Sometimes, sitting too much can make a problem called piles worse. Piles are like little lumps or bumps that can hurt or itch. If you sit down for too long, it can put pressure on these bumps.
Try to stand up and move around every hour. Go for a walk or stretch your legs. This can help you feel better.
If you can, use a cushion to sit on. It can make sitting more comfortable.
Sitting for a long time, especially on the toilet, can cause haemorrhoids. This happens because it puts extra pressure on the blood vessels in your bottom.
If you find it hard to read or understand this, you can use tools like text-to-speech apps. These apps can read the words out loud to you, which might help.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Evidence-Based Interventions: haemorrhoid surgery
Relevance: 100%
-
What can I do about haemorrhoids? | NHS
Relevance: 93%
-

Bleeding from the bottom rectal bleeding
Relevance: 41%
-
Bleeding from the bottom rectal bleeding
Relevance: 35%
-

What are the benefits of insoluble fiber?
Relevance: 30%
-

How does fiber benefit digestion?
Relevance: 26%
-

How does fiber benefit digestion?
Relevance: 20%
-

What is a fecal occult blood test?
Relevance: 19%
-

Can too much fiber be harmful?
Relevance: 15%
-

What are the symptoms of BPH?
Relevance: 14%
-

How to use the bowel cancer screening FIT kit | NHS
Relevance: 14%
-

What is Bowel Cancer?
Relevance: 14%
-

Is a colonoscopy necessary after a positive home test?
Relevance: 14%
-

How does a fecal occult blood test (FOBT) work?
Relevance: 12%
-
How to do the FIT bowel cancer screening test | Cancer Research UK
Relevance: 6%
-

How to treat constipation | NHS
Relevance: 6%
-

Is fibre good for health?
Relevance: 6%
-

Why is fiber important for gut health and aging?
Relevance: 6%


