
Find Help
More Items From Ergsy search
-
What's the difference between seminomas and non-seminomas?
Relevance: 100%
-

What is a seminoma?
Relevance: 55%
-
What is testicular cancer?
Relevance: 36%
-

What is the survival rate for testicular cancer?
Relevance: 35%
-

Can testicular cancer recur after treatment?
Relevance: 29%
-

What is testicular cancer?
Relevance: 25%
-

What types of treatments are available for testicular cancer?
Relevance: 23%
-

Is testicular cancer treatable?
Relevance: 21%
-

Can testicular cancer spread to other parts of the body?
Relevance: 20%
-

What role do tumor markers play in testicular cancer?
Relevance: 18%
The Basics of Germ Cell Tumours
Testicular cancer originates mainly from germ cells and is classified into two primary types: seminomas and non-seminomas. These types differ in various aspects such as growth patterns, age of onset, and treatment responses. Understanding the differences between these two can aid in better diagnosis and treatment of testicular cancer.
Characteristics of Seminomas
Seminomas are a type of germ cell tumour that generally occur in men between the ages of 25 and 45. They are known for their homogeneous structure and slower growth compared to non-seminomas. Seminomas usually have a better prognosis due to their responsiveness to radiation therapy. These tumours can be further categorised into classical seminomas, which are the most common, and spermatocytic seminomas, which typically occur in older men. A key feature of seminomas is their tendency to elevate levels of a marker called human chorionic gonadotropin (hCG) moderately, aiding in diagnosis.
Overview of Non-Seminomas
Non-seminomas are more diverse and tend to occur in younger men, usually between the ages of 15 and 35. They are more aggressive than seminomas and can rapidly spread to other parts of the body. Non-seminomas include various subtypes such as embryonal carcinoma, yolk sac tumour, choriocarcinoma, and teratoma. This group of tumours often requires more aggressive treatment, including combinations of surgery, chemotherapy, and rarely, radiation. Non-seminomas may produce elevated levels of both alpha-fetoprotein (AFP) and hCG, which are critical in their diagnosis and monitoring.
Key Differences in Treatment Approaches
One of the significant differences between seminomas and non-seminomas is their treatment protocols. Since seminomas respond well to radiation, this option is often part of their treatment plan alongside surgery. However, radiation is less effective against non-seminomas, which require chemotherapy along with surgical interventions. The choice of treatment depends on various factors including the stage of the cancer and patient-specific situations. Close monitoring through blood tests to check tumour markers and regular imaging scans are essential for both types.
Prognosis and Survival Rates
The prognosis for both seminomas and non-seminomas is generally good, especially when diagnosed early. Seminomas, due to their slower growth and increased sensitivity to radiation, have a slightly higher survival rate compared to non-seminomas. However, advances in chemotherapy have significantly improved the outcomes for patients with non-seminomas, achieving high overall survival rates. Active surveillance, careful monitoring, and timely treatment are crucial for effective management of both tumour types.
The Basics of Germ Cell Tumours
Testicular cancer starts in special cells called germ cells. There are two main types: seminomas and non-seminomas. They are different in how they grow, how old you are when you get them, and how they respond to treatments. Knowing these differences helps doctors diagnose and treat testicular cancer better.
Characteristics of Seminomas
Seminomas are a kind of germ cell tumour. They usually happen in men who are between 25 and 45 years old. They grow slowly and have a similar structure throughout. Seminomas are treated successfully with radiation. There are two types of seminomas: classical, which is the most common, and spermatocytic, found mainly in older men. Seminomas can cause an increase in a marker in the blood called hCG, which helps doctors diagnose them.
Overview of Non-Seminomas
Non-seminomas are more varied and usually happen in younger men, between 15 and 35 years old. They grow faster and can spread to other body parts quickly. Non-seminomas include types like embryonal carcinoma, yolk sac tumour, choriocarcinoma, and teratoma. They need strong treatments, using surgery and chemotherapy. Sometimes, radiation is used. Non-seminomas can raise markers in the blood called AFP and hCG, which are important for diagnosing and tracking them.
Key Differences in Treatment Approaches
Seminomas and non-seminomas have different treatments. Seminomas use radiation and surgery, as they respond well to radiation. Non-seminomas don’t respond well to radiation, so they need chemotherapy and surgery. Choosing the right treatment depends on things like how far the cancer has spread. Keeping an eye on cancer with blood tests and scans is important for both types.
Prognosis and Survival Rates
If found early, both seminomas and non-seminomas have a good chance of getting better. Seminomas have a slightly better survival rate because they grow slower and respond well to radiation. New treatments like chemotherapy have greatly improved survival rates for non-seminomas too. Watching closely, regular check-ups, and starting treatment quickly are key to managing both types of cancer effectively.
Frequently Asked Questions
What is the main difference between seminomas and non-seminomas?
The main difference is that seminomas are a type of germ cell tumor that generally grow more slowly and are more sensitive to radiation, whereas non-seminomas are a group of different types of tumors that tend to grow more quickly and are less sensitive to radiation.
Are seminomas more common than non-seminomas?
Seminomas and non-seminomas occur with roughly equal frequency overall, but the incidence can vary depending on age and demographic factors.
At what age do seminomas and non-seminomas typically occur?
Seminomas are more common in men in their 30s and 40s, while non-seminomas tend to occur in younger men, typically in their late teens to early 30s.
How are seminomas and non-seminomas diagnosed?
Diagnosis typically involves a physical exam, ultrasound of the testes, and blood tests for tumor markers. Histological examination of testicular tissue after removal of a testicular mass is required for definitive diagnosis.
What tumor markers are associated with seminomas and non-seminomas?
Seminomas may elevate levels of human chorionic gonadotropin (hCG) but not alpha-fetoprotein (AFP), whereas non-seminomas can raise levels of both hCG and AFP.
Are seminomas and non-seminomas treated differently?
Yes, seminomas are usually treated with radiation therapy and/or chemotherapy, while non-seminomas often require more aggressive chemotherapy regimens and might involve surgery.
Which has a better prognosis: seminomas or non-seminomas?
Seminomas generally have a better prognosis and a higher cure rate because they respond well to treatment, whereas the prognosis for non-seminomas depends on the specific type and stage.
Can both seminomas and non-seminomas spread to other parts of the body?
Yes, both types can metastasize, but the spread and patterns may vary. Non-seminomas tend to spread more quickly and aggressively than seminomas.
Are there subtypes within non-seminomas?
Yes, non-seminomas include several subtypes such as embryonal carcinoma, yolk sac tumor, choriocarcinoma, and teratoma.
How does the treatment duration differ for seminomas and non-seminomas?
Treatment duration can be longer for non-seminomas due to more intensive chemotherapy. Seminomas often require shorter, less intense treatment courses.
Do lifestyle factors influence the development of seminomas vs. non-seminomas?
While there are no specific lifestyle factors that determine if a person will develop seminomas or non-seminomas, risk factors such as undescended testicles and family history can influence the overall risk of testicular cancer.
Can both seminomas and non-seminomas recur after treatment?
Yes, both types can recur after treatment, but regular follow-up and monitoring can help manage and treat recurrences effectively.
Is fertility affected differently by seminomas and non-seminomas?
Both seminomas and non-seminomas can affect fertility due to the testes' involvement and side effects of treatment, but fertility preservation options are available.
Are imaging studies used differently for diagnosing seminomas vs. non-seminomas?
Imaging studies like CT scans and ultrasound are used for both; however, histological examination remains crucial for determining the specific type.
What is the role of surgery in the treatment of seminomas and non-seminomas?
Surgery, often an orchiectomy, is essential for both to remove the tumor. Additional retroperitoneal lymph node dissection may be more commonly performed for non-seminomas if needed.
How do seminomas and non-seminomas differ histologically?
Seminomas appear more uniform and are composed of large, round cells, while non-seminomas are more heterogeneous with various cell types depending on the subtype.
What is the typical stage at diagnosis for seminomas versus non-seminomas?
Seminomas are often diagnosed at an earlier stage due to slower growth and better predictability in symptoms, while non-seminomas may present at more advanced stages.
How does the response to chemotherapy differ for seminomas and non-seminomas?
Non-seminomas often require more aggressive multi-drug chemotherapy regimens, whereas seminomas typically respond well to standard chemotherapy treatments.
Can genetic factors influence the development of seminomas or non-seminomas?
Genetic factors, such as family history of testicular cancer, can increase risk, but specific genetic predispositions distinguishing seminomas from non-seminomas are not well-defined.
How important is follow-up care for patients with seminomas or non-seminomas?
Follow-up care is crucial for both types to monitor for recurrence, manage long-term treatment effects, and address any late-emerging complications.
What is the main difference between seminomas and non-seminomas?
Seminomas and non-seminomas are two types of testicular cancer. Here is how they are different:
- Seminomas grow slowly and can be treated easily.
- Non-seminomas grow faster and may need stronger treatment.
To help you understand better, you can:
- Ask someone to explain it to you in simple words.
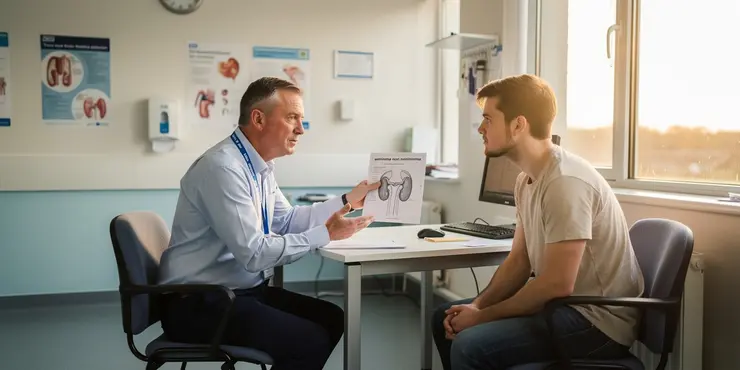
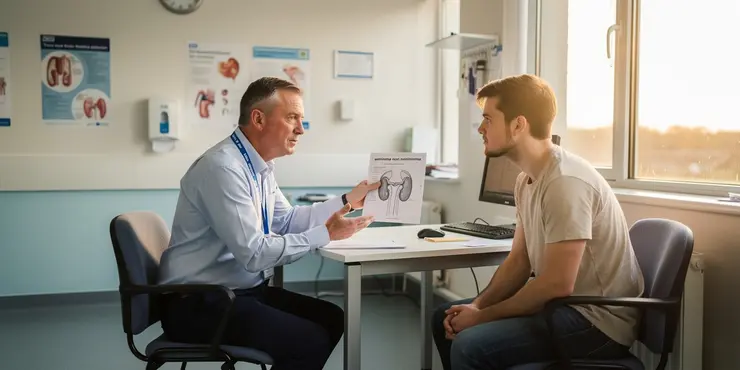
- Use pictures or drawings to see the difference.
- Use apps or tools that read the text out loud.
The big difference is that seminomas are a kind of germ cell tumor. They usually grow slowly and can be treated with radiation. Non-seminomas are a bunch of different tumors. They usually grow faster and are harder to treat with radiation.
Which is more common: seminomas or non-seminomas?
This question asks about two types of testicular cancer: seminomas and non-seminomas.
- Seminomas: A type of testicular cancer that grows slowly.
- Non-seminomas: A type of testicular cancer that can grow faster.
Support tools you can use:
- Pictograms: Use pictures to help understand the types of cancer.
- Read aloud: Use text-to-speech tools to listen while you read.
- Break it down: Focus on one sentence at a time to make it easier.
Remember, it's okay to ask someone to explain or help you understand more!
There are two main types of this health issue. They are called seminomas and non-seminomas. Both happen about the same amount of times. But, how often they happen can change. It depends on how old someone is and other things about them.
Helpful tools: You can use pictures or diagrams to help understand. Talking with a doctor or a nurse can also be good.
When do seminomas and non-seminomas usually happen?
Seminomas happen more often in men who are 30 to 40 years old. Non-seminomas usually happen in younger men, often in their late teens to early 30s.
How do doctors find out if someone has seminomas or non-seminomas?
To find out what's wrong, the doctor will look at your body. They will use a special camera, called an ultrasound, to look inside your testicles. They might also do a blood test to look for signs of a tumor.
If there's a lump in the testicle, it may need to be taken out so doctors can look carefully at it under a microscope. This helps them know for sure what it is.
What signs in the blood are linked to seminomas and non-seminomas?
Doctors look for special signs in the blood to help find and treat testicular cancer.
Sometimes, these signs can be different for two kinds of cancer called seminomas and non-seminomas.
If you need help reading:
- Ask someone to read this with you.
- Use a tool that reads text out loud.
- Highlight words you know to help understand the sentence.
Semenomas can make the hCG chemical go up, but not the AFP chemical. Non-seminomas can make both hCG and AFP go up.
Do doctors use different treatments for seminomas and non-seminomas?
There are two kinds of testicular cancer: seminomas and non-seminomas. They are both types of cancer that affect the male reproductive system. Doctors do use different treatments for each type.
Here is a simple way to understand this:
- Seminomas: These are usually treated with radiation or special medicine called chemotherapy.
- Non-seminomas: These might need surgery, and sometimes chemotherapy too.
If you're trying to understand more about this topic, you can:
- Use pictures or diagrams to visualize the treatments.
- Talk to a doctor or nurse who can explain things in a simple way.
- Look for videos or animations online that explain cancer and its treatments.
Yes, doctors often use special machines to kill cancer cells in seminomas. This is called radiation therapy. They might also use strong medicine called chemotherapy. Non-seminomas usually need even stronger chemotherapy. Sometimes, doctors need to do an operation to take out the cancer.
Which type is easier to treat: seminomas or non-seminomas?
Seminomas usually have a better chance of getting better because they react well to treatment. Non-seminomas might be different. It depends on the exact type and how much they have grown.
Can seminomas and non-seminomas move to other parts of the body?
Yes, both seminomas and non-seminomas can spread to other parts of the body. When cancer moves, it's called "spreading" or "metastasis".
Here are some tips to help understand:
- Break down words into smaller parts.
- Use a dictionary to look up tough words.
- Ask a grown-up or teacher for help.
Yes, both types can spread to other parts of the body. Non-seminomas spread faster and more aggressively than seminomas.
Are there different kinds of non-seminomas?
Yes, there are different kinds of non-seminomas. Some types are embryonal carcinoma, yolk sac tumor, choriocarcinoma, and teratoma.
Tip: Use a dictionary to help with hard words. Try reading out loud for extra help.
How long do treatments last for seminomas and non-seminomas?
Here is how to understand the length of treatment:
Seminomas: This is a kind of cancer. Treating seminomas usually takes a certain amount of time.
Non-seminomas: This is a different kind of cancer. Treating non-seminomas might take a different amount of time.
If you find reading hard, you can try using simple tools like picture aids or audiobooks. They can help make the information clearer and easier to understand.
Treatment time can be longer for non-seminomas because the medicine is stronger and takes longer to work. Seminomas usually need a shorter time with less strong treatment.
Do the things we do every day change the chances of getting seminomas or non-seminomas?
This question asks if everyday habits, like how we eat or exercise, change the chances of getting seminomas or non-seminomas. Seminomas and non-seminomas are types of testicular cancer.
Tools to help you understand:
- Use a dictionary to check any hard words.
- Ask an adult to explain any parts you find tricky.
- Draw pictures to help remember the information.
There are no exact things in your life that will say if you will get seminomas or non-seminomas, which are types of testicular cancer. But some things can make it more likely, like if your testicles didn't drop down when you were a baby or if someone in your family had it.
You can try some tools to help learn more, like asking a doctor or using websites that explain things simply.
Can seminomas and non-seminomas come back after treatment?
Yes, both seminomas and non-seminomas can come back after being treated. It's important to have regular check-ups with your doctor. This helps to catch any signs early if the cancer returns.
To make reading easier, you can:
- Use a highlighter to mark important words.
- Ask someone to read it with you.
- Use pictures or drawings to help understand the words.
Yes, both kinds can come back after treatment. But going to the doctor often and checking regularly can help find and treat them if they come back. It's like having a plan to make sure everything is okay.
Do seminomas and non-seminomas change fertility in different ways?
There are two types of these conditions. They are called seminomas and non-seminomas. Both can make it hard to have children. This is because they affect the testes and the treatments can have side effects. But there are ways to protect your ability to have children.
Do doctors use different scans for seminomas and non-seminomas?
Doctors use special pictures called CT scans or ultrasound to look inside the body. But, to find out exactly what something is, doctors need to look at it under a microscope.
How does surgery help treat seminomas and non-seminomas?
Surgery is important to take out the tumor. This surgery is often called an orchiectomy. Sometimes, doctors also need to take out some lymph nodes from inside the belly. They do this more often for a type of tumor called non-seminomas if they need to.
What is the difference between seminomas and non-seminomas under a microscope?
Seminomas have cells that look the same. They are big and round. Non-seminomas have different kinds of cells that can look different. The way they look can change based on the type.
When do doctors usually find seminomas and non-seminomas?
Seminomas are usually found early because they grow slowly and have clearer signs. Non-seminomas might be found later because they grow faster.
How do seminomas and non-seminomas respond differently to chemotherapy?
Chemotherapy is a strong medicine that fights cancer. There are two main types of testicular cancer: seminomas and non-seminomas. They react differently to this medicine.
Seminomas:
Seminomas usually respond well to chemotherapy. This means the medicine often works to make the cancer smaller or go away.
Non-seminomas:
Non-seminomas may not respond as well. Doctors might need to use stronger chemotherapy or different treatments to help.
If you find reading hard, ask someone you know to read with you. Using pictures can also help you understand better.
There are two types of cancer we are talking about: non-seminomas and seminomas.
Non-seminomas need strong medicine that uses more than one drug to fight the cancer.
Seminomas usually get better with regular cancer medicine.
If reading is hard, you can ask someone to help read aloud. You can also use apps that read text for you. Pictures and charts can help understand better too.
Can genes affect the growth of seminomas or non-seminomas?
Genes are like instructions in your body. They help decide how your body grows and works.
Sometimes, genes can change in a way that is not normal. This can help some types of lumps, called seminomas and non-seminomas, to grow.
If you want to learn more, it can be helpful to talk to a doctor. They can give you good advice and support to understand better.
If people in your family have had testicular cancer, you might have a higher chance of getting it too. We don’t know exactly which genes make seminomas different from non-seminomas.
Why is follow-up care important for people with seminomas or non-seminomas?
Follow-up care means going back to the doctor after your main treatment.
This is important to check that the cancer has not come back.
It helps doctors see if you need more treatment.
You should always go to your follow-up appointments.
It can make you feel better and keep you healthy.
Using a calendar or reminder on your phone can help you remember your appointments.
It is very important to go back to the doctor after your main treatment. This is to check if the illness comes back, to help with any long-term effects, and to take care of any new problems that might show up later.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-
What's the difference between seminomas and non-seminomas?
Relevance: 100%
-

What is a seminoma?
Relevance: 55%
-
What is testicular cancer?
Relevance: 36%
-

What is the survival rate for testicular cancer?
Relevance: 35%
-

Can testicular cancer recur after treatment?
Relevance: 29%
-

What is testicular cancer?
Relevance: 25%
-

What types of treatments are available for testicular cancer?
Relevance: 23%
-

Is testicular cancer treatable?
Relevance: 21%
-

Can testicular cancer spread to other parts of the body?
Relevance: 20%
-

What role do tumor markers play in testicular cancer?
Relevance: 18%




