Find Help
More Items From Ergsy search
-

Greater trochanteric pain syndrome
Relevance: 100%
-

Social Prescribing in Greater Manchester
Relevance: 26%
-

Exercises for sciatica: piriformis syndrome | NHS
Relevance: 25%
-

Carpal Tunnel Syndrome
Relevance: 24%
-

Is chronic fatigue syndrome contagious?
Relevance: 23%
-

What is Cushing's syndrome?
Relevance: 22%
-

Munchausen's syndrome | NHS
Relevance: 22%
-

What are the common symptoms of Carpal Tunnel Syndrome?
Relevance: 22%
-

What is Carpal Tunnel Syndrome (CTS)?
Relevance: 22%
-

Are there any alternative treatments for Carpal Tunnel Syndrome?
Relevance: 22%
-

Having a child with Down's syndrome | NHS
Relevance: 22%
-

Prader-Willi Syndrome | NHS
Relevance: 22%
-

What causes Carpal Tunnel Syndrome?
Relevance: 22%
-

Symptoms of irritable bowel syndrome (IBS)
Relevance: 21%
-
What is chronic fatigue syndrome?
Relevance: 21%
-
How can I prevent Carpal Tunnel Syndrome?
Relevance: 21%
-

How is Carpal Tunnel Syndrome diagnosed?
Relevance: 21%
-
Is chronic fatigue syndrome a mental illness?
Relevance: 21%
-

Are there specific exercises that can help with Carpal Tunnel Syndrome?
Relevance: 21%
-

Is Carpal Tunnel Syndrome covered by the NHS?
Relevance: 21%
-

What non-surgical treatments are available for Carpal Tunnel Syndrome?
Relevance: 21%
-
Why is there a call for greater transparency in banking fees?
Relevance: 21%
-

Turner syndrome: Beyond the classic XO phenotype
Relevance: 20%
-

Shoulder subacromial shoulder pain
Relevance: 20%
-

Calls for Greater Transparency in Banking Fees as Complaints Rise
Relevance: 20%
-

When should I consider surgery for Carpal Tunnel Syndrome?
Relevance: 20%
-

Down's syndrome: Emily's story | NHS
Relevance: 20%
-

Is a mammogram painful?
Relevance: 20%
-
Can Carpal Tunnel Syndrome recur after treatment?
Relevance: 20%
-

What is complex sleep apnea syndrome?
Relevance: 20%
-
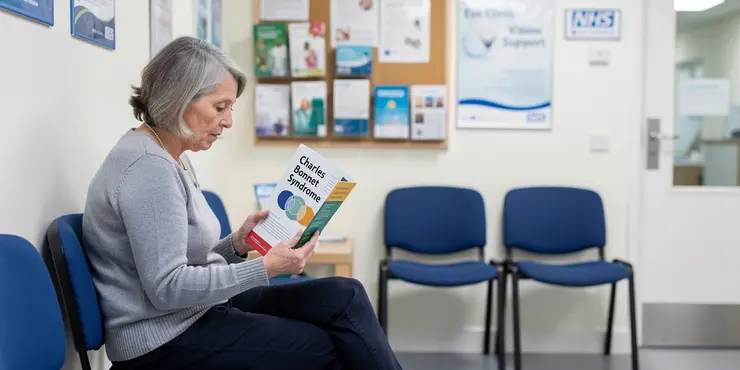
Charles Bonnet Syndrome
Relevance: 20%
-

Diagnosing irritable bowel syndrome (IBS)
Relevance: 20%
-

What causes chronic fatigue syndrome?
Relevance: 20%
-

About irritable bowel syndrome (IBS)
Relevance: 20%
-

About irritable bowel syndrome (IBS)
Relevance: 20%
-

What is irritable bowel syndrome (IBS)?
Relevance: 20%
-
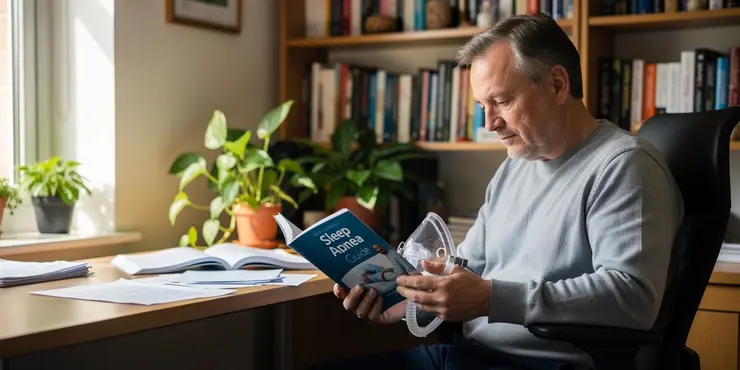
What is complex sleep apnea syndrome?
Relevance: 20%
-

How is chronic fatigue syndrome treated?
Relevance: 20%
-
Can children develop chronic fatigue syndrome?
Relevance: 19%
-

Treating irritable bowel syndrome (IBS)
Relevance: 19%
Greater Trochanteric Pain Syndrome
What is Greater Trochanteric Pain Syndrome?
Greater Trochanteric Pain Syndrome (GTPS) is a medical condition that causes pain in the outer part of the hip, specifically the greater trochanter area of the femur (thigh bone). The term 'Trochanteric Bursitis' was previously used to describe this condition, but it is now understood to involve more than just bursitis, including tendinopathy and muscle tears. GTPS predominantly affects middle-aged women and can significantly impact mobility and quality of life.
Causes of GTPS
Several factors can contribute to the development of GTPS, including:
- Overuse Injuries: Repetitive motion or prolonged pressure on the hip area can lead to tendon and bursa inflammation.
- Muscle Imbalances: Weakness or tightness in the hip muscles can alter normal gait and add stress to the tendon attachments.
- Trauma: A direct blow to the hip or falling on the hip can result in inflammation.
- Biomechanical Issues: Abnormalities in the way you walk or run can predispose you to GTPS.
Symptoms of GTPS
People with GTPS typically experience the following symptoms:
- Pain: Persistent pain on the outside of the hip, which may radiate down the outside of the thigh.
- Tenderness: Tenderness around the greater trochanter when pressing on the hip.
- Swelling: Possible swelling or warmth over the lateral hip region.
- Pain at Night: Pain may worsen at night or when lying on the affected side.
- Limited Range of Motion: Difficulty or discomfort with movements such as walking, climbing stairs, or sitting cross-legged.
Diagnosis
Diagnosing GTPS typically involves a thorough clinical evaluation by a healthcare provider. They may review your medical history, perform a physical examination focusing on the hip area, and assess your gait. Additionally, imaging studies such as X-rays, ultrasound, or MRI may be requested to rule out other conditions and confirm the diagnosis.
Treatment Options
GTPS is usually manageable with a combination of the following treatments:
- Rest and Activity Modification: Avoiding activities that exacerbate symptoms and allowing time for healing.
- Physical Therapy: A focused exercise programme to strengthen hip muscles, improve flexibility, and correct biomechanical issues.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce pain and inflammation.
- Injections: Corticosteroid injections can provide temporary relief from pain and inflammation.
- Extracorporeal Shock Wave Therapy (ESWT): A non-invasive treatment using shock waves to promote healing.
- Surgery: Rarely needed, but may be considered in severe or refractory cases.
Prevention
To prevent GTPS, consider adopting the following lifestyle modifications:
- Maintain a Healthy Weight: Reducing excess weight can lessen the stress on your hips.
- Exercise Regularly: Engage in a balanced exercise routine that includes strength training, stretching, and aerobic activities.
- Proper Footwear: Wear supportive shoes that align well with your gait and activity levels.
- Avoid Overuse: Gradually increase activity intensity and duration to avoid overstressing your hip muscles.
- Good Posture: Maintain proper posture during activities to ensure even distribution of body weight.
Greater Trochanteric Pain Syndrome
What is Greater Trochanteric Pain Syndrome?
Greater Trochanteric Pain Syndrome (GTPS) is a condition that causes pain on the outside of the hip. This pain happens at a part of the thigh bone called the greater trochanter. It can affect how you move and affect your daily life. It mostly affects women who are middle-aged.
Causes of GTPS
Many things can cause GTPS, like:
- Overuse Injuries: Doing the same motion over and over or putting pressure on the hip can cause damage.
- Muscle Imbalances: When hip muscles are too weak or too tight, it can change how you walk and hurt the hip area.
- Trauma: Getting hit hard on the hip or falling can cause pain and swelling.
- Biomechanical Issues: Unusual ways of walking or running can lead to GTPS.
Symptoms of GTPS
People with GTPS usually have these symptoms:
- Pain: Pain on the outside of the hip that might go down the outside of the thigh.
- Tenderness: The hip feels sore when touched.
- Swelling: Swelling or warmth on the side of the hip.
- Pain at Night: Pain can be worse at night or when lying on the painful side.
- Limited Range of Motion: Trouble moving, walking, climbing stairs, or sitting with legs crossed.
Diagnosis
To find out if you have GTPS, a doctor will check your hip and ask about your health history. They might also use X-rays or do a scan to make sure it's GTPS and not something else.
Treatment Options
You can often manage GTPS in these ways:
- Rest and Activity Modification: Take breaks from activities that cause pain and let your hip heal.
- Physical Therapy: Exercises to make hip muscles stronger and more flexible.
- Medications: Pills to help with pain and swelling.
- Injections: Shots that can reduce pain for a while.
- Extracorporeal Shock Wave Therapy (ESWT): A treatment with shock waves to help healing.
- Surgery: Rarely needed, only if other treatments do not work.
Prevention
To help prevent GTPS, try to:
- Maintain a Healthy Weight: Keeping a proper weight can reduce stress on your hips.
- Exercise Regularly: Do exercises for strength, stretching, and heart health.
- Proper Footwear: Wear good shoes that support your feet.
- Avoid Overuse: Increase how much you move or exercise slowly to avoid hurting your hips.
- Good Posture: Stand and sit in a balanced way to spread your body weight evenly.
Frequently Asked Questions
What is Greater Trochanteric Pain Syndrome (GTPS)?
Greater Trochanteric Pain Syndrome (GTPS) is a condition characterized by pain and tenderness on the outer side of the hip, usually related to inflammation or injury to the muscles, tendons, or bursae in the area.
What are the common symptoms of GTPS?
Common symptoms include pain on the outside of the hip and thigh, tenderness over the greater trochanter, discomfort when lying on the affected side, and pain that worsens with activity such as walking or climbing stairs.
What causes GTPS?
GTPS can be caused by overuse or repetitive activities, trauma to the hip, muscle tears, tendon degeneration, or bursitis. It is also sometimes associated with conditions such as iliotibial band syndrome or osteoarthritis.
Who is at risk for developing GTPS?
People at risk include those who engage in repetitive hip movements, runners, individuals with a high body mass index (BMI), women, and those aged between 40 and 60 years.
How is GTPS diagnosed?
A GP or specialist typically diagnoses GTPS through a physical examination, patient history, and sometimes imaging tests such as ultrasound or MRI to rule out other conditions.
What are the initial treatments for GTPS?
Initial treatments often include rest, ice application, anti-inflammatory medications, and physical therapy aimed at strengthening and stretching the hip muscles.
Are there specific exercises that help with GTPS?
Yes, exercises that focus on strengthening the hip abductors, such as side leg lifts, and stretching the iliotibial band can be beneficial. A physiotherapist can provide a tailored exercise programme.
Can I still exercise if I have GTPS?
Yes, but it's important to modify activities to avoid those that exacerbate pain. Low-impact activities like swimming or cycling may be more suitable while the condition heals.
How long does it take for GTPS to heal?
The recovery time can vary, but with proper treatment, many people start to see improvement within a few weeks to a few months. Persistent cases may take longer to resolve.
Is surgery ever required for GTPS?
Surgery is rarely needed for GTPS and is typically considered only when conservative treatments fail over a long period. Surgery might involve tendon repair or bursectomy.
Can GTPS recur after treatment?
Yes, GTPS can recur, especially if the underlying causes are not addressed. Maintaining strong and flexible hip muscles, and avoiding repetitive hip strain, can help prevent recurrence.
Are there any lifestyle changes that can help manage GTPS?
Yes, maintaining a healthy weight, practicing good posture, using ergonomically designed furniture, and avoiding activities that strain the hip can help manage and prevent GTPS.
Can GTPS be prevented?
While not all cases can be prevented, reducing risk factors such as avoiding repetitive hip movements and maintaining proper hip strength and flexibility can reduce the likelihood of developing GTPS.
Is GTPS related to hip arthritis?
GTPS can coexist with hip arthritis but they are distinct conditions. Hip arthritis involves joint degeneration while GTPS involves inflammation or injury to the surrounding tendons or bursae.
Should I see a specialist for GTPS?
If initial treatments by a GP do not improve symptoms, or if the pain is severe, seeing a specialist such as an orthopaedic surgeon or a physiotherapist may be beneficial for further management.
What is Greater Trochanteric Pain Syndrome (GTPS)?
Greater Trochanteric Pain Syndrome (GTPS) is a condition that causes pain on the side of your hip. It can make moving your hip hurt.
If you have GTPS, you might feel sore, stiff, or have trouble walking. Sometimes, it hurts more when you lie on one side.
It can help to see a doctor if you think you have GTPS. The doctor can help you feel better.
To help, you can use soft pillows to sit or sleep. Rest and gentle stretches might also help your hip feel better.
Greater Trochanteric Pain Syndrome (GTPS) is when your hip hurts on the outside. It happens because the muscles or the bits that attach them are sore or hurt.
What signs show you might have GTPS?
Some common signs are hip and thigh pain on the side, a sore spot on the hip, feeling uncomfortable when lying down on the sore side, and pain that gets worse when you move, like walking or going up stairs.
What makes GTPS happen?
GTPS stands for Greater Trochanteric Pain Syndrome. This is a long name for pain on the outside of your hip.
Here are some things that can make GTPS start:
- Doing too much exercise.
- Falling down or hurting your hip.
- Having tight muscles or weak muscles.
- Standing or sitting in one way for too long.
If you think you have GTPS, it can help to:
- Rest your hip.
- Use ice packs on your hip.
- Talk to a doctor or a therapist.
- Do gentle stretches.
These things can help make your hip feel better.
GTPS can hurt your hip because of doing the same activity too much, hurting your hip, or tearing a muscle. It can also happen if a tendon gets weak or if you have swelling in a small sack near your hip. GTPS can also be linked to other problems like a tight band in your leg or joint pain from getting older.
To help understand better, you can use pictures or videos. Breaking information into small steps can help too.
Who might get GTPS?
People who might have problems:
- People who move their hips a lot.
- People who run.
- People who have a bigger body size.
- Women.
- People aged between 40 and 60 years old.
To help understand, you can use pictures or get a friend to explain more.
How do doctors find out if someone has GTPS?
Doctors use a few steps to see if a person has GTPS. Here is what they do:
- Ask Questions: The doctor will ask how you feel and what hurts.
- Check Your Hip: The doctor will touch and move your hip to see where it hurts.
- Pictures of Your Hip: Sometimes, doctors take pictures of your hip using machines like X-ray or MRI. This helps them see inside.
If you have trouble reading, you can ask someone to read it with you. Using pictures can also help you understand better.
A doctor checks for GTPS by looking at how your hip feels and moves. They ask about your health and any pain you have. Sometimes they use special pictures like ultrasound or MRI to make sure it's not something else.
What can help with GTPS at the start?
Here are some simple ways to feel better:
- Rest: Take breaks and don't do things that hurt.
- Ice: Put a cold pack on the sore area for 15 minutes.
- Pain Medicine: Ask an adult if you can have medicine to help with the pain.
- Stretches: Do gentle exercises to make your muscles feel better.
- Talk to a Doctor: A doctor can tell you the best ways to get better.
You can try these things at home. A grown-up or doctor can help you with these steps.
First treatments might be:
- Resting your hip.
- Putting ice on your hip to make it feel better.
- Taking medicine to help with swelling and pain.
- Doing exercises to make your hip stronger and more flexible.
Ask a doctor or therapist for help with these treatments.
What exercises can help with GTPS?
Here are some exercises that might help:
- Leg lifts: Lie on your side and lift your leg up and down slowly.
- Bridges: Lie on your back with your knees bent. Lift your hips up to make a bridge shape.
- Wall slides: Stand against a wall and slide down like you are sitting in an invisible chair.
These exercises can help make your muscles stronger.
If you need help, ask a parent or a teacher. You can also try watching videos to see how to do these moves.
Yes, doing exercises to make your hip muscles stronger can help. Try side leg lifts. Stretching the long band on the side of your leg is good too. A physiotherapist can give you exercises that are right for you.
Can I still do exercise if I have GTPS?
GTPS is a problem with your hip. You might feel pain on the side of your hip.
You can still do some exercises, but you need to be careful. Ask a doctor or a physio for help. They can show you safe exercises.
You can try easy activities like walking or swimming. These are gentle on your hips.
Listen to your body. If something hurts, stop and rest.
Tools like heat packs or ice can help if you have pain. Use them on your hip.
Yes, you can still do things, but make sure they don't make your pain worse. Try gentle activities like swimming or riding a bike. These are softer on your body while you heal.
How long does it take for GTPS to get better?
GTPS is a problem with your hip. Healing time is different for everyone.
Getting better can take a few weeks to a few months.
Here are some tips to help:
- Rest your hip.
- Use ice packs on your hip for 15-20 minutes.
- Talk to a doctor or therapist for help.
How fast you get better can change. But with the right help, many people start feeling better in a few weeks or months. Sometimes it can take longer.
Do you ever need surgery for GTPS?
GTPS means Greater Trochanteric Pain Syndrome. It's a problem with the hip.
Most people don't need surgery for GTPS. Doctors usually try other treatments first, like:
- Resting the hip
- Doing special exercises
- Taking medicine to help with pain
If these treatments don't help, a doctor might talk to you about surgery.
It's important to see a doctor if your hip hurts a lot.
Tools that can help:
- Talk to a doctor or nurse if you have questions
- Ask someone you trust to come with you to appointments
- Use pictures or drawings to understand better
Surgery is not often needed for GTPS. Doctors usually think about surgery only if other treatments don't work after a long time. Surgery might fix tendons or remove a bursa.
Can GTPS come back after getting better?
Yes, GTPS can come back, especially if we don't fix the reasons why it happened. Keeping hip muscles strong and stretchy, and not using the hip too much, can help stop it from coming back.
Can changes in daily habits help with GTPS?
Yes. Changing some things in your day-to-day life can help with GTPS.
- Stay active: Move your body gently, like walking or swimming.
- Rest: Take breaks and avoid doing too much.
- Healthy food: Eat vegetables, fruits, and other good foods.
- Talk to a doctor: A doctor can give you good advice.
- Use ice packs: Putting ice on sore areas can help.
Here are some tools that can help:
- Use a cane: This can help when walking.
- Wear good shoes: Shoes that fit well can stop pain.
- Pain creams: These can help make pain less.
Yes, keeping a healthy weight, sitting up straight, using comfy chairs and desks, and not doing things that hurt the hip can help with GTPS.
Can we stop GTPS from happening?
There are some things we can't stop. But we can do things that might help. We can try not to move our hips the same way too much. We can also make our hips strong and stretchy. This can help us not get GTPS.
Tools that can help:
- Follow exercises to make your hips strong.
- Make your hips flexible with stretching activities.
- Use videos to see how to move your hips safely.
Does GTPS have anything to do with hip arthritis?
GTPS stands for Greater Trochanteric Pain Syndrome. It's a condition that can cause pain on the side of your hip.
Hip arthritis is when the joints in your hip get worn out, and it can also cause pain.
If you have hip pain and want to know more, talk to your doctor. They can help you understand what's happening.
To help with reading:
- You can use audiobooks or read out loud.
- Ask someone to explain any tricky words.
- Use pictures to help understand the words.
GTPS and hip arthritis can happen together, but they are not the same. Hip arthritis means the hip joint is wearing out. GTPS means the parts around the hip, like tendons or bursae, are hurt or swollen.
Do I need to see a doctor for GTPS?
If your first treatments by a doctor do not help, or if the pain is very bad, it might help to see a specialist. You can see a bone doctor or a physiotherapist for more help.
Useful Links
This website offers general information and is not a substitute for professional advice.
Always seek guidance from qualified professionals.
If you have any medical concerns or need urgent help, contact a healthcare professional or emergency services immediately.
Some of this content was generated with AI assistance. We’ve done our best to keep it accurate, helpful, and human-friendly.
- Ergsy carfully checks the information in the videos we provide here.
- Videos shown by Youtube after a video has completed, have NOT been reviewed by ERGSY.
- To view, click the arrow in centre of video.
- Most of the videos you find here will have subtitles and/or closed captions available.
- You may need to turn these on, and choose your preferred language.
- Go to the video you'd like to watch.
- If closed captions (CC) are available, settings will be visible on the bottom right of the video player.
- To turn on Captions, click settings .
- To turn off Captions, click settings again.
More Items From Ergsy search
-

Greater trochanteric pain syndrome
Relevance: 100%
-

Social Prescribing in Greater Manchester
Relevance: 26%
-

Exercises for sciatica: piriformis syndrome | NHS
Relevance: 25%
-

Carpal Tunnel Syndrome
Relevance: 24%
-

Is chronic fatigue syndrome contagious?
Relevance: 23%
-

What is Cushing's syndrome?
Relevance: 22%
-

Munchausen's syndrome | NHS
Relevance: 22%
-

What are the common symptoms of Carpal Tunnel Syndrome?
Relevance: 22%
-

What is Carpal Tunnel Syndrome (CTS)?
Relevance: 22%
-

Are there any alternative treatments for Carpal Tunnel Syndrome?
Relevance: 22%
-

Having a child with Down's syndrome | NHS
Relevance: 22%
-

Prader-Willi Syndrome | NHS
Relevance: 22%
-

What causes Carpal Tunnel Syndrome?
Relevance: 22%
-

Symptoms of irritable bowel syndrome (IBS)
Relevance: 21%
-
What is chronic fatigue syndrome?
Relevance: 21%
-
How can I prevent Carpal Tunnel Syndrome?
Relevance: 21%
-

How is Carpal Tunnel Syndrome diagnosed?
Relevance: 21%
-
Is chronic fatigue syndrome a mental illness?
Relevance: 21%
-

Are there specific exercises that can help with Carpal Tunnel Syndrome?
Relevance: 21%
-

Is Carpal Tunnel Syndrome covered by the NHS?
Relevance: 21%
-

What non-surgical treatments are available for Carpal Tunnel Syndrome?
Relevance: 21%
-
Why is there a call for greater transparency in banking fees?
Relevance: 21%
-

Turner syndrome: Beyond the classic XO phenotype
Relevance: 20%
-

Shoulder subacromial shoulder pain
Relevance: 20%
-

Calls for Greater Transparency in Banking Fees as Complaints Rise
Relevance: 20%
-

When should I consider surgery for Carpal Tunnel Syndrome?
Relevance: 20%
-

Down's syndrome: Emily's story | NHS
Relevance: 20%
-

Is a mammogram painful?
Relevance: 20%
-
Can Carpal Tunnel Syndrome recur after treatment?
Relevance: 20%
-

What is complex sleep apnea syndrome?
Relevance: 20%
-
Charles Bonnet Syndrome
Relevance: 20%
-

Diagnosing irritable bowel syndrome (IBS)
Relevance: 20%
-

What causes chronic fatigue syndrome?
Relevance: 20%
-

About irritable bowel syndrome (IBS)
Relevance: 20%
-

About irritable bowel syndrome (IBS)
Relevance: 20%
-

What is irritable bowel syndrome (IBS)?
Relevance: 20%
-
What is complex sleep apnea syndrome?
Relevance: 20%
-

How is chronic fatigue syndrome treated?
Relevance: 20%
-
Can children develop chronic fatigue syndrome?
Relevance: 19%
-

Treating irritable bowel syndrome (IBS)
Relevance: 19%


